Experimental Modeling to Clarify Speech Disorders Due to VPI
Velopharyngeal insufficiency (VPI) affects 30% of children with structural abnormalities of the oral and nasal cavities.1-3 In the majority of cases where VPI is caused by cleft palate, the VPI persists despite the surgical repair. (Approximately 4,200 babies are born annually with cleft lip and cleft palate.4) The aim of a new study being conducted at University of Cincinnati (UC) Medical Center and Cincinnati Children’s Hospital Medical Center – the only center in the country conducting such research – is to demonstrate that a less than total closure of the velopharyngeal port post-surgery is insufficient to address the patient’s speech disorders. Led by Liran Oren, PhD, research assistant professor, department of otolaryngology, the study will explore the mechanisms of voice and speech disorders. Using experimental and computational modeling, Dr. Oren hopes to demonstrate that even small openings in the velopharyngeal port after surgery can cause significant speech disorders.
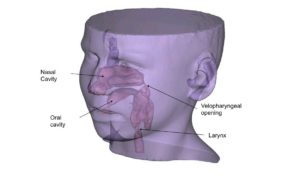
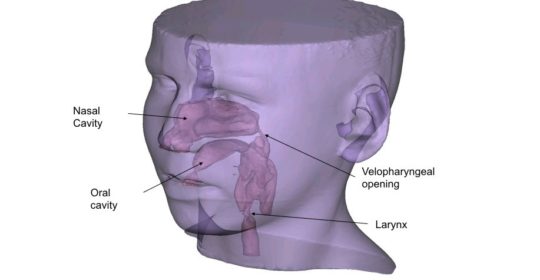
An image showing an example for the computational model used in the study. The geometry of the airway is reconstructed from CT scans of a patient with VPI.
Image courtesy of Liran Oren, PhD
Speech disorders due to VPI result from the incomplete surgical closing of the VP opening between the oral and nasal cavities. This condition can lead to hypernasality (too much sound reverberating in the nasal cavity during speech), nasal air emission (air leakage through VP valve), and abnormal speech formation. The current standard for surgical intervention assumes that the severity of speech caused by VPI is associated with the degree of VP opening. Yet, according to Dr. Oren, “clinicians have noted a lack of correlation between the size of the VP opening and the severity of speech disorder.” The study outcomes will help clinicians predict how different surgical procedures can affect quality of speech.
In Dr. Oren’s six-patient study, three patients, who have been diagnosed with hypernasality and a large VP opening, will undergo scans of the upper airway and the pharynx. “I can adjust the scans after they are digitized,” Dr. Oren said, “to shrink the upper airway, pharynx, and opening to simulate how air flow will affect patients with nasal emission.” In the second stage of the study, three patients diagnosed with nasal emission and a small opening will also be scanned, and Dr. Oren will experiment with the digitized images of these scans. He anticipates that the qualities of air flow and acoustics can be modified to mirror the characteristics of hypernasal patients. Dr. Oren hypothesizes that the relationship between acoustics (that characterize hypernasality) and the size of the opening, and aeroacoustics (that characterize nasal emission) and the size of the opening will be inverse to each other.
This study is funded by the National Institutes of Health Mentored Quantitative Research Career Development Awards K25 program, which provides grants for up to five years for study and research by professionals who are transitioning from a science/technology/engineering/mathematics environment to medicine.5 Among other topics in his training program, Dr. Oren, an aerospace engineer, will study speech pathology in preparation for the study.
References
1. Phua YS, de Chalain T. Incidence of oronasal fistulae and velopharyngeal insufficiency after cleft palate repair: an audit of 211 children born between 1990 and 2004. Cleft Palate Craniofac J. 2008;45:172-178.
2. Inman DS, Thomas P, Hodgkinson PD, Reid CA. Oro-nasal fistula development and velopharyngeal insufficiency following primary cleft palate surgery—an audit of 148 children born between 1985 and 1997.Br J Plast Surg. 2005;58:1051-1054.
3. Sullivan SR, Marrinan EM, LaBrie RA, Rogers GF, Mulliken JB. (2009). Palatoplasty outcomes in nonsyndromic patients with cleft palate: a 29-year assessment of one surgeon’s experience. J Craniofac Surg. 2009;20:1629-1630.
4. Cleft lip and cleft palate. March of Dimes. Available at: http://www.marchofdimes.org/baby/cleft-lip-and-cleft-palate.aspx. Accessed June 20, 2016.
5. Mentored quantitative research career development awards (K25). National Institute of General Medical Sciences. Available at: https://www.nigms.nih.gov/training/careerdev/Pages/MentoredQuantRes.aspx. Accessed June 20, 2016.
Additional Resources
Biavati MJ, Rocha-Worley G, Wiet GJ. Velopharyngeal insufficiency. Medscape. Available at: http://emedicine.medscape.com/article/873018-overview. Accessed June 20, 2016.
Kummer AW. Resonance disorders & velopharyngeal dysfunction: assessment and intervention. Speech-Language Pathology. Cincinnati Children’s Hospital. Available at: http://www.cincinnatichildrens.org/service/s/speech/hcp/lecture-notes/. Accessed June 20, 2016.
 Liran Oren, PhD
Liran Oren, PhD
Research Assistant Professor
Department of Otolaryngology
University of Cincinnati College of Medicine
Phone: (513) 558-0073
E-mail: orenl@ucmail.uc.edu
Leave a reply →

