Intensive Training in Allergy Treatment Modalities Facilitates Administration of Sublingual Immunotherapy (SLIT)
Sublingual immunotherapy (SLIT) involves dosing the allergen under the tongue of the patient in controlled amounts, often over a period of several years, in order to increase tolerance to a particular allergen and diminish symptoms brought on by exposure to that allergen.1 SLIT using aqueous drops has been used sporadically in the United States since its discovery by French Hansel, MD, in St. Louis in the 1920s. For the last 30 years, it has been in wider clinical use in numerous countries in Europe and Australasia to treat allergies. A surge of research regarding efficacy and safety in the last five to ten years led to United States Food & Drug Administration (FDA) approval of the soluble tablet formulation in 2014. The University of Cincinnati Medical Center Otolaryngic Allergy Program staff is well-prepared to use this newly-approved technique due to the extensive training they have received.
Following a rigorous allergy treatment algorithm, the process begins with a detailed clinical history of the patient, combined with skin and/or serum testing to determine specific elevations in immunoglobulin E (IgE), indicating allergen sensitivities and their intensity. Alfred Sassler, DO, Associate Professor of Otolaryngology, directs the Allergy Program at the University of Cincinnati Medical Center, and trains the clinical staff personally. He is one of very few physicians in the region who have demonstrated the knowledge and experience to attain the status of Fellow in the American Academy of Otolaryngic Allergy (AAOA). He adds, “All of our allergy nurses attend an intensive training program conducted by the AAOA. Their participation is not required by the profession, but we believe that better-informed and trained staff can better treat our patients.” The multi-day AAOA training program centers around clinical issues related to the care of allergy/immunology and inflammatory diseases of the airways and systems related to the head and neck.2 It is structured as a continuing education course for physicians (otolaryngologists and others), PA/NPs, and allied health staff who support their physicians in the management of allergic patients. The course also provides face-to-face opportunities with expert faculty to answer clinical questions and hands-on workshops to demonstrate and hone technical skills.2
Sassler spearheaded the development of the allergy program upon his arrival in 2011, and as of today, the practice is a robust and growing one, which uses approximately half subcutaneous delivery and half sublingual delivery for its immunotherapy patients. SLIT has been rigorously vetted and is shown to be safe and effective for the treatment of the allergic rhinitis and conjunctivitis symptoms that are often seen with seasonal allergies. It has shown promise in recent studies for improvement with the often associated and growing problem of asthma. It is frequently administered in academic medical centers, in large part due to the influence and involvement of the AAOA. Sassler emphasizes the vital role of the primary care setting, however, he maintains, “Due to the rapidly increasing number of allergy cases, primary care providers are treating a much higher volume of these patients than they did in the past, and these clinicians need to be educated about the advanced therapies available through specialists when avoidance, environmental controls and pharmacotherapy are inadequate.”
Standardized dosing of sublingual immunotherapy remains an area of intense study, and many variables influence efficacy of allergy immunotherapy for subcutaneous as well as sublingual administration. Read more.
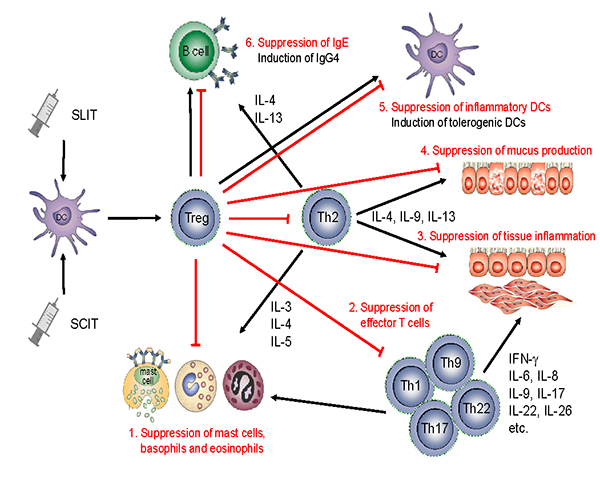
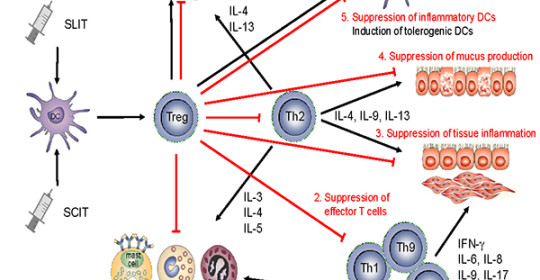
Mechanisms of allergen-specific immunotherapy and the role of regulatory T cells in allergic diseases.
An allergen is taken up by regional dendritic cells leading to the induction of regulatory T cells. These cells suppress allergic responses directly and indirectly by the following mechanisms. 1. Suppression of mast cells, basophils and eosinophils. 2. Suppression of effector T cells. 3. Suppression of inflammatory cell migration to tissues and tissue inflammation. 4. Suppression of mucus production. 5. Suppression of inflammatory dendritic cells and induction of tolerogenic dendritic cells. 6. Suppression of allergen-specific IgE and induction of IgG4 from B cells. Reference: Fujita et al. Clinical and Translational Allergy 2012 2:2 doi:10.1186/2045-7022-2-2
 Alfred Sassler, DO, FAAOA, FACS
Alfred Sassler, DO, FAAOA, FACS
Associate Professor of Otolaryngology
Medical School: Philadelphia College of Osteopathic Medicine
(606) 584-0841
sasslea@ucmail.uc.edu

