“I knew when I woke up that morning, that day was going to be my last,” said UC Health Transplant patient Barry Johnson, as he recalls the night before he received a phone call that would save his life.
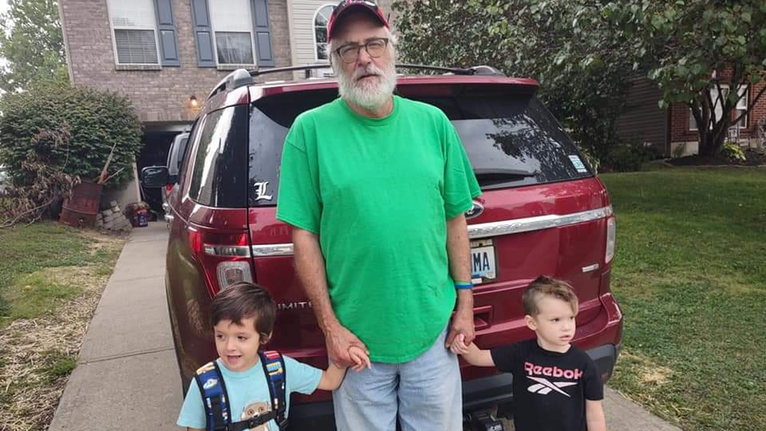
Barry is a 62-year-old widowed father of one and a grandfather. His hobbies include collecting and breeding tropical fish, restoring old cars, creative writing and sharing his transplantation story with anyone who might benefit from it.
While his main career prior to the decline of his condition in 2018 was as a social worker and social work professor, since the surgery, he has returned to work part time doing “fun kinds of jobs,” like working for the Cincinnati Reds as an usher and CVG Airport helping disabled people board and exit planes safely.
Today, Barry is healthy for the first time since he was 22 years old.
Diagnosis, Remission and Finding UC Health
“I’ve been sick all my life. And I guess when you’re sick, you just don’t realize what that means to be healthy,” said Barry.
It was the summer after he graduated college when his healthcare journey began. He was diagnosed with a rare autoimmune disorder called sarcoidosis. This is a disease that can affect any organ in the body, causing inflammation of the body tissues, and ultimately, preventing oxygen from reaching organs. And in Barry’s case, it was his liver.
At the time of his diagnosis, he recalls the doctors not being hopeful that he would have a long life.
“Basically, they told me back in the early 80’s that transplant would be the only thing that could save my life. But they just weren’t doing them. They were doing some, but they were risky and not a lot of people survived them,” he explained.
After being told this, he put the idea of transplant in the back of his head. He would occasionally keep up with what was going on with transplant on the news and popular media, but that was about it.
“But honestly, I never thought I would live to be the age where I would need a liver transplant. I never thought I would survive past my 40’s,” said Barry.
His sarcoidosis went into remission, and Barry was both shocked and relieved that he was doing better.
“There was nobody really in Louisville, where I lived at the time, that knew how to treat it, so I did a little research and found that one of the world experts was at UC Health—just 100 miles away,” he said.
At this point, Barry packed up his life, took a job near Cincinnati as one of his first jobs in social work and began seeing Robert Baughman, MD, UC Health pulmonologist and professor in the Department of Internal Medicine at the University of Cincinnati College of Medicine. Dr. Baughman has been treating him for 40 years now, and outside of his clinical work, his research interests include the diagnosis and treatment of patients with sarcoidosis.
“Sarcoidosis can affect many parts of the body, including the lungs, eyes, heart and brain. In Barry's case, his liver was attacked and the scarring as a result of the inflammation eventually led to enough cirrhosis that he needed a transplant,” Dr. Baughman explained.
Hope for a Future
While under Dr. Baughman’s care, Barry’s condition remained in remission, and he recalls how he began to be hopeful as he continued to improve. Other than getting easily fatigued, he hardly showed any symptoms.
It wasn’t until 1999, at 40 years old, the age he never thought he would make it past, that it dawned on Barry that he could have a future.
“That’s when I first started thinking about it. I guess when you’re so young and you have a diagnosis like that, I never thought of getting married and having a wife and kids because I thought I had an expiration date,” he goes on to explain. “It didn’t make sense to subject anyone to watch me die, basically.”
So, he met his wife, got married and not long after, adopted their daughter, Megan.
At this point, things were looking up for Barry and stayed that way for a while. It wasn’t until 2013 that his condition began to decline once again.
Barry began to experience rupturing of the veins in his throat, something he explains to be common with liver disease.
“My wife and daughter were always very concerned about my condition, particularly when it started declining in 2013. While my wife was alive, she was worried and scared, but she was hopeful,” he said.
After several emergency hospital visits for ruptured veins, transplant was once again mentioned and brought to the forefront of his mind. But this time, it began being seriously discussed.
“Dr. Baughman started talking to me about the same thing. He and my gastrointestinal doctors were on the same page. He told me, ‘We have an excellent transplant program right here at UC Health—basically across the hall. I want to refer you over there,’” Barry recalled.
After Dr. Baughman’s referral, Barry was contacted by UC Health Transplant and brought in for several days of testing and was accepted as a patient.
“I remember the very first serious conversation I had about transplant. I guess you just don’t believe it. Transplants are pretty common now, but if you really think about what happens in a transplant surgery, it is nothing short of a miracle,” he said.
Waiting for “The Call”
On Dec. 20, 2018, Barry Johnson was officially put on the transplant waiting list.
“It was hell. There’s no other way to put it. It’s hard to describe waiting by the phone for a call that will save your life,” he explained.
He recalls a point in the summer of 2019, just several months after being put on the transplant waiting list, where every day he could measure how much worse he had become by the things he could no longer do. In these moments, he was feeling as though he was a “passive observer” to his own death, as all he could do was wait and hope.
In addition to the physical trauma of his declining condition, Barry explains that he struggled through a lot of pre-surgery emotional struggles.
“You’ve probably heard of people going through survivors’ guilt and all of that stuff, and I guess I got into some of that. You know like, ‘What makes me worthy of receiving something like this?’’’ he explained.
Throughout a pre- and post-transplant journey, it is critical for transplant patients to have a solid support system. This is something that UC Health Transplant understands very well.
While Barry’s wife was no longer alive to see him work with the transplant center, his daughter, Megan, was there every step of the way and truly enabled him to survive during the toughest of times.
Along with Megan’s support, Barry worked with Alexandra Gee, PsyD, UC Health psychologist and assistant professor in the Department of Psychiatry & Behavioral Neuroscience at the UC College of Medicine, who is specifically trained to work with transplant patients. Dr. Gee helped him to reframe his thinking and helped him in using a much more positive frame of mind.
In addition to family and expert psychological support, Barry was assigned a nurse coordinator who would call him every week to remind him that they were all thinking of him.
“My nurse coordinator, Travis, would call and tell me, ‘We haven’t given up,’ and that I was at the top of their list to talk about in every meeting,” Barry said. “In the back of my mind, I thought, ‘Yeah, he’s just a compassionate guy and just trying to give me a sense of hope,’ but evidently, he did mean it because I eventually got that call.”
“Barry was one of those few unfortunate patients with end-stage liver disease whose MELD score was incongruent with the symptoms he was experiencing on a daily basis,” explained Travis Doty, RN, Barry’s assigned nurse coordinator.
A model for end-stage liver disease (MELD) score is a figure that determines the severity of a patient’s liver disease. The score can fluctuate from six to 40 based on the patient’s condition and helps clinicians determine how quickly a patient needs a liver transplant.
“Barry struggled daily with encephalopathy, or confusion,” said Travis. “He would sometimes forget conversations that we had a few days prior, so many of our conversations centered on keeping his spirits up and keeping him motivated.”
The Phone Rings
In January 2020, Barry contracted a fungal infection in his throat. He explained that when your health declines, you become more susceptible to more ailments. At this point, a common cold would have hospitalized him.
He was hospitalized with this infection for about a month, and when it came time for him to be discharged, he had the distinct feeling that he was being sent home to die.
He went home, planned his funeral and sold many of his items, as he did not want to let that fall on his daughter.
On the morning of March 10, 2020, Barry woke up and knew that would be his last day alive.
“I don’t know how I knew this, and I don’t know how to describe it, but I knew that day was going to be the day that I die. I just knew it. I had never felt that way before, I just knew it,” he said.
At this point, knowing what he knew, he made the decision that if he were to die, he was not going to do it at home. He did not want his daughter to find him like that.
“I decided to go to a high school basketball game. How I got there, I don’t know, but I did. And I was sitting in the gym watching this basketball game when my phone starts ringing,” he explained.
The call came from an unknown number, so he ignored it. But then the number called again, and the phone rang and rang and rang. Annoyed, Barry picked up the phone and answered the call. On the other end of the phone was his transplant surgeon’s assistant telling him to get to the hospital right now. They had a liver for him.
“I was very surprised by how quick things happened once I got to the hospital,” he said.
In 20 minutes, Barry found himself walking through the doors of UC Medical Center, and 40 minutes later, he was on his way to the operating room. His daughter was the last face he saw before his liver transplant.
Barry’s life was changed in a matter of hours. His surgery was performed by Shimul A. Shah, MD, UC Health transplant surgeon and the James and Catherine Orr Endowed Chair of Liver Transplantation, Director of the Division of Transplantation and professor in the Department of Surgery at the UC College of Medicine; as well as Latifa Silski, MD, UC Health kidney and liver transplant surgeon and assistant professor in the Department of Surgery at the UC College of Medicine.
“I remember that so clearly, waking up that morning and just knowing that without a doubt, that day was my last day. And in a way it was. That was my last day as a dying man and the next day, I was better,” said Barry.
A New Life and New Hope
“It’s nothing short of a miracle. I would’ve died sometime that month, there’s no doubt, the doctors even told me that,” he said.
After struggling and fighting for his health for so long, Barry now lives a healthy life and is grateful for the hope that got him through every day before the surgery.
“If I die tomorrow, if I got hit by a bus or something, I’ll die a happy person. Every day is a blessing, I get to see my grandkids, I get to spend more time with my daughter, I get to share my story, I get to instill hope in other people. It’s nothing short of a miracle,” he said.
In recovery, he recalls the impact every person involved in his care at UC Health made on him. From the environmental services staff, to the nurses and doctors. He felt as though every person at UC Health understands what trauma patients are going through and the healing that they need.
“While the cornerstone of every good transplant program is its commitment to a multidisciplinary approach, I do believe our team is truly exceptional. The kind of dedication and level of expertise from each team member, not only on their best days, but also on their worst, really makes lifesaving transplants possible,” Dr. Silski explained. “Surgery is one part of the process in bringing a second chance at life, and I am grateful for the team that revolves around the patient from the moment of their referral to long after the successful transplant.”
This is something Barry echoes as he recalls his treatment from start to finish.
“To me, it was all around hope,” said Barry. “I know that’s the motto of UC Health—In Science Lives Hope. For me, hope is everything, and as long as I had hope, I felt like I could face any obstacle. There were times I didn’t have it, and I never want to go back to those days again.”
“As a matter of fact, one of the first things that the UC Health Transplant team told me was that they were never going to give up,” Barry continued. “UC Health gave me hope.”