The UC Esophageal Disease Center is the region’s only team of experts that subspecialize in the treatment of esophageal diseases and esophageal cancer. World-class care is delivered by subspecialists from thoracic surgery, surgical oncology, gastroenterology, medical oncology and radiation oncology as well as a full support team of nurses and ancillary professionals. We promise our expertise in esophageal disorders, delivering hope right here in Cincinnati.
Gastroesophageal Reflux Disease (GERD)
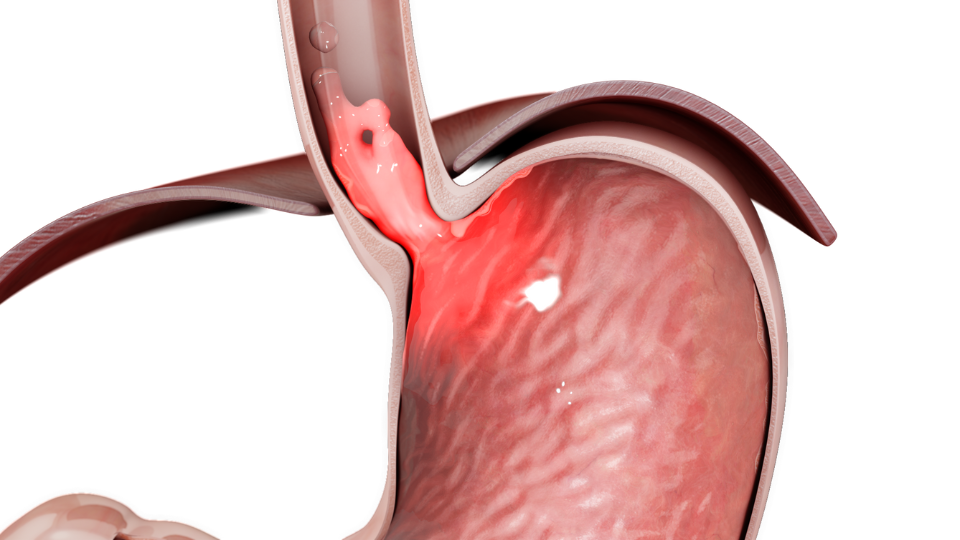
Gastroesophageal Reflux Disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (the esophagus). This backwash (acid reflux) can irritate the lining of your esophagus, leading to GERD.
Our Capabilities
Our Esophageal Disease experts are a multidisciplinary team focused on providing personalized, comprehensive care. Our collaborative process allows us to provide the right approach for your needs – across both nonsurgical and surgical options.
Compassionate Healing Starts Here
Click below to learn more about where you can find compassionate care.
ABOUT THIS CONDITION
Understanding Gastroesophageal Reflux Disease
Introduction to GERD
Gastroesophageal Reflux Disease (GERD) is more than just occasional heartburn; it's a persistent condition that affects millions worldwide. While many experience the occasional discomfort of acid reflux after a heavy meal, GERD is characterized by frequent and severe episodes that can significantly impact quality of life.
This comprehensive guide delves into the nuances of GERD, distinguishing it from occasional acid reflux, and lays the groundwork for understanding its causes, symptoms, and the wide array of treatment options available. By shedding light on this common yet often misunderstood condition, we aim to empower individuals with the knowledge to identify symptoms early, seek appropriate medical advice, and navigate the path to effective management and relief. Join us as we explore the complexities of gastroesophageal reflux disease, offering insights into how this condition affects the esophagus, the potential complications, and the importance of a tailored approach to treatment and lifestyle adjustments for long-term management.
Understanding the Basics of GERD
What is GERD?
Gastroesophageal Reflux Disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (the esophagus). This backwash (acid reflux) can irritate the lining of your esophagus, leading to GERD. Unlike occasional acid reflux, which many people experience without major issues, GERD is characterized by frequent and severe acid reflux, often leading to more serious health problems if left untreated.
Causes and Risk Factors
The root cause of GERD is a weak or relaxed lower esophageal sphincter (LES). This ring of muscle acts as a valve between your esophagus and stomach. When it functions properly, it prevents the backward flow of stomach contents. However, if the LES weakens or relaxes abnormally, acid can flow back into the esophagus, causing GERD. Factors that can contribute to this condition include obesity, certain foods and beverages, smoking, pregnancy, and a hiatal hernia—a condition where part of the stomach moves above the diaphragm.
Symptoms of GERD
GERD symptoms vary in frequency and intensity, but the most common include:
- Heartburn: A burning discomfort or pain that may move from your stomach to your abdomen or chest, or even up into your throat.
- Regurgitation: A sour or bitter-tasting acid backing up into your throat or mouth.
- Chest pain: Often confused with heart attack pain, particularly when it occurs after eating.
Less common symptoms can include difficulty swallowing, chronic cough, a sensation of a lump in the throat, and new or worsening asthma. If you experience persistent or severe symptoms of GERD, it's crucial to consult a healthcare provider to prevent potential complications.
The Impact of GERD on the Esophagus
Chronic exposure to stomach acid can lead to several complications within the esophagus, including:
- Esophagitis: Inflammation that can damage tissues of the esophagus.
- Esophageal Strictures: The narrowing of the esophagus, which can interfere with swallowing.
- Barrett's Esophagus: A serious condition where the tissue lining the esophagus changes, becoming more like the tissue that lines the intestine. This can increase the risk of developing esophageal cancer.
Understanding the severity of these complications underscores the importance of managing GERD symptoms through lifestyle changes, medication, or surgery, as recommended by healthcare professionals.
Diagnosing GERD
The journey to a definitive GERD diagnosis often begins with a detailed medical history and a physical examination conducted by a healthcare professional. When symptoms suggest GERD, further tests may be recommended to confirm the diagnosis and assess the severity of the condition.
Common Diagnostic Tests
- Upper Endoscopy: A procedure where a thin, flexible tube with a light and camera (endoscope) is used to examine the inside of your esophagus and stomach. This can help identify any esophageal damage or other related conditions.
- Esophageal pH Monitoring: A test that measures the amount of acid in your esophagus over a 24-hour period, providing detailed information about acid reflux incidents.
- Esophageal Manometry: Measures the rhythmic muscle contractions in your esophagus when you swallow and the coordination and force exerted by the esophagus muscles.
These diagnostic tools play a critical role in determining the presence and extent of GERD, guiding the healthcare provider in recommending the most appropriate treatment plan.
Treatment Options for GERD
Managing GERD effectively requires a comprehensive approach that may include lifestyle modifications, medications, or in some cases, surgery. The goal of treatment is to relieve symptoms, manage complications, and prevent reflux.
Lifestyle Modifications
Simple changes in daily habits can significantly alleviate GERD symptoms:
- Avoid foods and drinks that trigger reflux, such as fatty foods, coffee, and alcohol.
- Eat smaller, more frequent meals instead of large meals.
- Maintain a healthy weight to reduce pressure on the stomach and LES.
- Elevate the head of your bed to prevent nighttime symptoms.
- Quit smoking, as it can weaken the LES.
Medication
Various over-the-counter and prescription medications can reduce or block acid production and help heal the esophagus:
- Antacids: Provide quick relief by neutralizing stomach acid.
- H2 Receptor Blockers: Reduce acid production. While not as fast-acting as antacids, their effects last longer.
- Proton Pump Inhibitors (PPIs): The most effective medications for reducing stomach acid, helping to heal the esophagus.
Surgical and Other Procedures
For those who don't respond to medication or have severe GERD, surgery might be an option:
- Nissen Fundoplication: A surgical procedure that wraps the top of the stomach around the lower esophagus to tighten the LES and prevent reflux.
- LINX Device: A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus to strengthen the LES, preventing reflux while allowing food to pass.
- TIF Procedure: A minimally invasive GERD treatment, eliminates the need for abdominal incisions, offering quicker recovery and reduced risks. It's a significant leap in addressing chronic acid reflux by rebuilding the anti-reflux barrier.
Living with GERD: Management and Coping Strategies
Living with GERD involves more than just treating symptoms; it's about adopting a lifestyle that supports digestive health and minimizes reflux episodes. Here are some strategies:
- Monitor Symptoms: Keeping a food and symptom diary can help identify triggers and the effectiveness of treatments.
- Stress Management: Stress can exacerbate GERD symptoms. Techniques like meditation, yoga, and deep breathing can help manage stress levels.
- Consult Healthcare Providers Regularly: Ongoing communication with healthcare providers is essential to adjust treatments as needed and to monitor for potential complications.
Living with GERD can be challenging, but with the right management strategies and support from healthcare professionals, individuals can lead full and active lives without letting GERD define them.
Help Along the Way
Answers to your Questions about GERD
Occasional acid reflux is common and usually occurs after eating certain foods or large meals. GERD, however, involves frequent and severe acid reflux that can lead to complications if untreated.
Yes, simple lifestyle adjustments like dietary changes, weight management, and avoiding trigger foods can greatly reduce GERD symptoms for many individuals.
Chronic, untreated GERD can lead to esophagitis, Barrett's esophagus, esophageal strictures, and even esophageal cancer.
GERD is diagnosed through a combination of medical history, physical examination, and specialized tests such as upper endoscopy, esophageal pH monitoring, and esophageal manometry.
Treatment options include lifestyle modifications, medications (antacids, H2 receptor blockers, proton pump inhibitors), and surgical procedures for severe cases.
Surgery can effectively manage GERD symptoms and repair anatomical issues, but it's generally considered after other treatments have failed and not necessarily a cure for everyone.
Certain foods and beverages can trigger GERD symptoms by relaxing the lower esophageal sphincter or irritating the esophagus. Identifying and avoiding these triggers can help manage symptoms.
The lower esophageal sphincter (LES) acts as a valve preventing backflow of stomach contents. GERD occurs when the LES is weak or relaxes inappropriately, allowing acid to reflux into the esophagus.
Conditions like hiatal hernia, Barrett's esophagus, and esophageal cancer can be related to or exacerbated by GERD.
Effective management involves a combination of dietary changes, lifestyle modifications, medication as prescribed by a healthcare provider, and in some cases, surgical interventions.
Contact Us
At UC Health, we lead the region in scientific discoveries and embrace a spirit of purpose – offering our patients and their families something beyond everyday healthcare. At UC Health, we offer hope.