The pathology frozen room on the second floor of University of Cincinnati Medical Center is much smaller than its neighboring operating rooms.
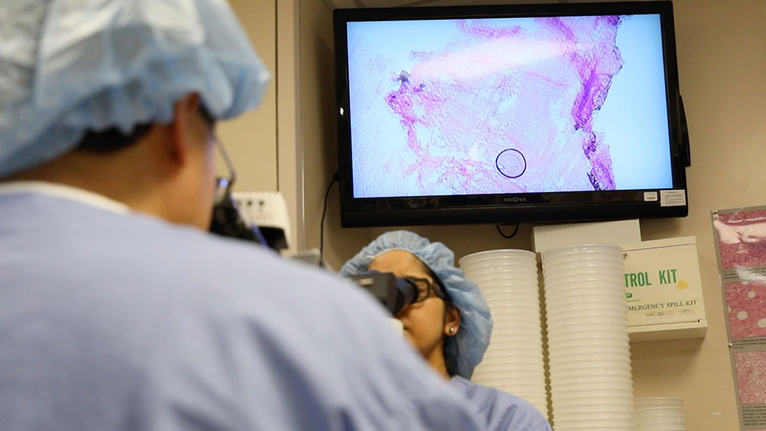
There is enough space for one or two people to stand at a counter as they slice through specimens, dip slides in dye or receive fresh tissue at the window from a nurse in the middle of a surgery.
But the role of pathology on this floor is far from small—what pathologists see under their microscopes can make the difference in what happens next for patients.
“In the public, most people don’t know what we in pathology do,” said Jiang Wang, MD, PhD, chief of anatomic pathology and director of surgical pathology for the UC College of Medicine. “But we really play a very key role, especially for cancer patients.”
Pathologists are trained to identify and diagnose diseases from the body’s tissues and organs, often at microscopic levels. What may look like scattered purple and pink dots to others looks like a high-grade malignant tumor to a pathologist.
These physicians, whose work happens backstage from clinic rooms and hospital beds, confirm suspected diagnoses and then some. They deliver key details that can mean all the difference to a patient’s care.
While pathologists still must interpret what they see, the truth is right in front of them. The cells don’t lie.