Assessment and Management of CSF Leaks Is Individualized at UC Medical Center
Physicians at the University of Cincinnati (UC) Medical Center individualize the management of temporal bone spontaneous cerebrospinal fluid (CSF) leaks for each patient. Kareem O. Tawfik, MD, otology fellow, department of otolaryngology – head and neck surgery at UC Health, said that the process begins with establishing the diagnosis, which typically involves beta-2 transferrin testing and imaging to identify the potential site of the leak within the temporal bone. A tympanostomy tube is often placed to facilitate collection of a sample of the patient’s ear discharge. Patients can often collect the discharge in a test tube at home, and the results are available several days after the sample is sent for laboratory analysis.
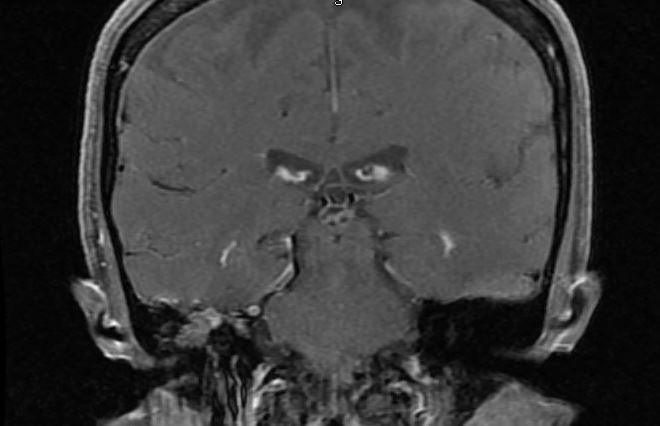
This image shows a coronal T1 post-contrast fat saturated MRI image of a right temporal bone meningoencephalocele. Image courtesy of Kareem O. Tawfik, MD.
Computed tomography (CT) and/or magnetic resonance imaging (MRI) are routinely performed to localize the defect in the skull base and to rule out any associated mass lesions or destructive processes. CT scans “are excellent in revealing bony dehiscences of the skull base, whereas MRI provides superior soft-tissue detail and can detect the presence or absence of associated meningoceles/encephaloceles,” he said. Lumbar puncture is also commonly performed to detect underlying idiopathic intracranial hypertension. The association between idiopathic intracranial hypertension and CSF leaks is increasingly being recognized, and management of underlying intracranial hypertension is important to minimize patients’ risk of future CSF leaks. Patients with intracranial hypertension are at greater risk of future CSF leaks; these patients experience a gradual erosion of the skull base (and ultimately, the dura mater).
Surgical management decisions depend on factors such as suspected site of the leak (ie, lateral versus medial), unifocality versus multifocality of skull base defects, presence or absence of intracranial hypertension, primary versus recurrent nature of the problem and the nature of the hearing loss. “Generally speaking, a lateral, unifocal temporal bone CSF leak may be amenable to repair via a transmastoid approach, whereas multifocal, medial or large temporal bone CSF leaks may require middle fossa craniotomies. In many cases, we prepare patients for both approaches, and obtain consent for both, and then begin surgery with a transmastoid approach. When this is successful, we can avoid performing a craniotomy,” Dr. Tawfik said. The decision to subject patients to lumbar drainage in the postoperative period depends on surgeon discretion, but this may be advisable in patients with known elevated intracranial pressure or in whom a previous attempt at repair of a CSF leak has failed. Obliterative procedures, in which the mastoid and/or middle ear are filled with soft tissue, bone, or other materials, can also be considered, particularly for patients in whom a leak cannot be localized intraoperatively or who have failed previous interventions. These procedures are often performed with concomitant Eustachian tube obliteration and blind sac closure of the external auditory canal.
Adjunctive diagnostic measures may include radionuclide cisternography, MR or CT cisternograms, and injection of intrathecal substances to facilitate with diagnosis either by imaging or before exploratory surgery.
“We have a robust experience with evaluation and management of spontaneous CSF leaks, and we are seeing increasing numbers of patients with these problems at UC Medical Center,” Dr. Tawfik said. “UC Health is uniquely equipped to address these complex issues, owing to a team of highly skilled neurotologists, neurosurgeons, neurologists and neuroradiologists. As practitioners in an academic health system, we hold monthly multidisciplinary conferences to discuss how best to manage patients immediately and in the long term.” Many patients with spontaneous CSF leaks have risk factors for recurrence. Some patients with refractory idiopathic intracranial hypertension may require lumboperitoneal shunts. Recurrence of CSF leaks is uncommon after surgical intervention, however, these patients require close, coordinated, long-term follow-up to minimize the likelihood of recurrence.
 Kareem O. Tawfik, MD
Kareem O. Tawfik, MD
Otology Fellow
Department of Otolaryngology – Head & Neck Surgery
UC Health
tawfikkm@UCMAIL.UC.EDU
(513) 475-8000
UCHealth.com

