Exploring a Novel Method for Improving Facial Nerve Healing from Facial Nerve Injury
A facial nerve injury results in significant functional deficits and cosmetic deformities. Better methods are still needed to improve facial nerve healing resulting from injuries.1 To further explore this clear need to improve facial nerve healing, a team at the University of Cincinnati Medical Center examined the use of magnesium filaments to assist in peripheral nerve healing. David Hom, MD, Director, Division of Facial Plastic and Reconstructive Surgery in the Department of Otolaryngology at UC Medical Center and Matt Hershcovitch, MD, former otolaryngology resident collaborated with Sarah Pixley, PhD, University of Cincinnati Department of Molecular and Cellular Physiology to develop this novel idea, which was nationally recognized with an AAO-HNS research grant by the American Academy of Otolaryngology Head and Neck Surgery (AAO-HNS) and the American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS) Leslie Bernstein Resident Research Grant.
Recently, the preliminary results of this research were published in the Journal of Biomaterials Applications and the new method of using MicroCT to analyze the biomaterial filaments was highlighted in the Journal of Neuroscience Methods.2,3 The collaborators have seen encouraging results in utilizing magnesium as a method to help improve closing the nerve gap of peripheral nerve injuries to help these patients heal more completely.
Specifically, biodegradable magnesium metal filaments were placed inside biodegradable nerve conduits to attempt to provide the physical guidance and support to aid in the regeneration of peripheral nerves across injury gaps in a rodent model. At six weeks after implantation, magnesium degradation was examined by micro-computed tomography and histological analyses.
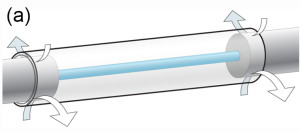
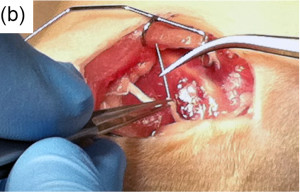
Surgery: (a) a scaffold diagram (arrows=sutures), (b) surgical pictures of the Mg insertion into nerve at surgery and (c) the PCL conduit in place.
Mg: magnesium; PCL: poly(caprolactone).2
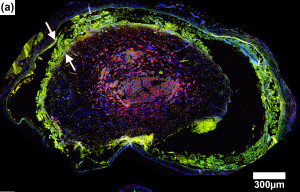
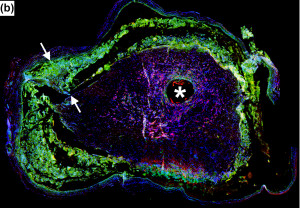
Using histological and immunocytochemical analyses, good biocompatibility of the magnesium implants was observed, with good development of regenerating nerve mini-fascicles and only mild inflammation in tissues even after complete degradation of the magnesium.
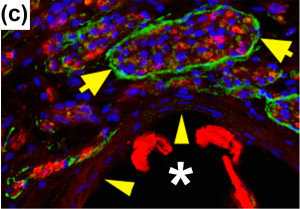
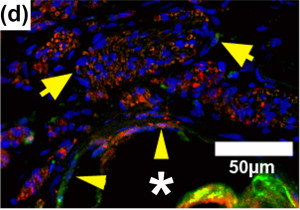
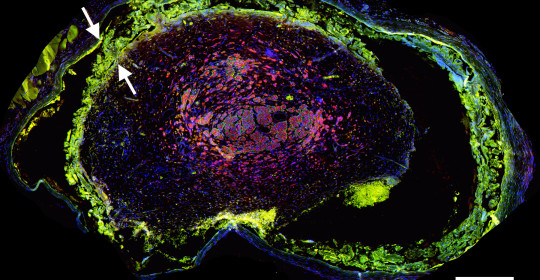
Figures A-D: Immunostained regenerating tissues after 6 weeks; (a and b) mid-conduit sections were stained for GLUT1 (green)/S100 (red)/DAPI (blue) in (a) NoMgSa and (b) MgSa animals (*cavity left by Mg, arrows delineate conduit material, bar=300μm). (c and d) Regenerating nerve mini-fascicles, indicated by arrows, run close to the Mg cavities, which are marked by * and arrowheads. The same staining was done on the section in (c), while the section in (d) was stained with ED1 (green)/NF200 (red)/DAPI (blue). Note GLUT1þ perineurium in (c) and thin layer of ED1+ macrophages above arrowheads in (d) (bar in c and d=50μm).
NoMgSa: saline filler only; MgSa: saline and Mg; GLUT1: glucose transporter 1; DAPI: 4’ 6-diamidino-2-phenylindole.2
Reproduced by permission of SAGE Publications Ltd., London, Los Angeles, New Delhi, Singapore and Washington DC.
In the current state, the need for improved facial nerve healing is exemplified by the following patient, a 44-year-old female with a spontaneous history of bilateral facial paralysis with slow facial nerve healing over three years, giving her a longstanding residual facial paresis of the lower face. Three years later, she had persistent bilateral decreased lower lip competence resulting in drooling, and the inability to smile. The patient required bilateral staged temporalis muscle slings to improve her lower facial support, lip competence and facial movement. The possibility exists that intervention with magnesium filaments could one day circumvent the need for facial reconstructive surgery such as the procedures done to improve this patient’s function.

Figure 1a Preoperative state, resting
44-year-old female with a history of initial bilateral facial paralysis with slow facial nerve healing resulting in longstanding residual facial paresis of lower face. Three years later, she still has persistent bilateral decreased lower lip competence when eating and speaking with drooling and the inability to smile.

Figure 2a Postoperative state (one year later), resting
She underwent bilateral staged temporalis muscle slings to improve her lower facial support, lip competence and facial movement to control her drooling and allow her to smile.
Challenging cases such as this example were recently presented at the National AAO- HNS meeting in Dallas 2015 by Hom and Ravi Samy, MD. Over the last seven years, Drs. Hom and Samy have taught an annual National AAO-HNS course on “Optimal Surgical Strategies for Treating Facial Paralysis” from a facial plastic surgery and neurotology standpoint.4 Continued research into magnesium filament implants, which have the potential to improve repair of injured peripheral nerve defects, may help improve outcomes in these patients. Says Hom, “Our study is preliminary research, but the findings are promising, and seem to indicate that magnesium is compatible with peripheral nerve healing. Clearly, this warrants additional study.”
References:
1.Hom DB, Reanimation of the Paralyzed Face. Clinical Otology. (Eds Pensak M, Choo D) Thieme, 2014
2.Vennemeyer J, Hopkins T, Hershcovitch M, Little K, Hagen M, Minteer D, Hom D, Marra K, Pixley S. Initial observations on using magnesium metal in peripheral nerve repair. J Biomater Appl 2015;29(8):1145-54. 2.
3.Hopkins TM, Heilman AM, Liggett JA, LaSance K, Little KJ, Hom DB, Minteer DM, Marra KG, Pixley SK. Combining micro-computed tomography with histology to analyze biomedical implants for peripheral nerve repair. J Neurosci Methods 2015;255:122-130.
4. Hom DB, Samy R. AAO-HNS Course, Optimal Surgical Strategies for Treating Facial Paralysis. Dallas, Sept 2015.

David Hom, MD
Director, Division of Facial Plastic and Reconstructive Surgery
Department of Otolaryngology – Head and Neck Surgery
Phone: (513) 558-3552
Email: homdb@ucmail.uc.edu
Connect with David Hom, MD on Doximity