UC Health Digestive Diseases is one of the oldest and most distinguished programs in the nation. We specialize in the areas of gastroenterology, hepatology and liver transplant medicine.
Inflammatory Bowel Disease (IBD)
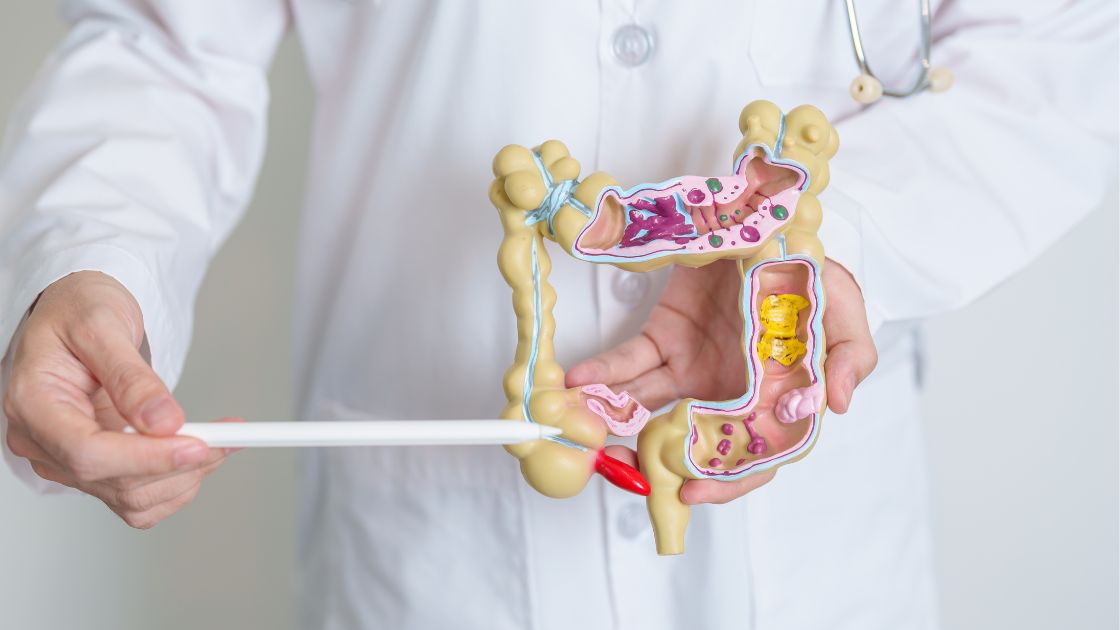
Inflammatory Bowel Disease (IBD) represents a group of conditions characterized by chronic inflammation in the digestive tract. The two main forms of IBD are ulcerative colitis and Crohn's disease, both of which affect the body in different ways.
Our Capabilities
Our team offers a multidisciplinary approach to the management of IBD – which includes IBD specialized gastroenterologists, advanced practice providers, pharmacists, dietitians, mental health specialists and more. Our specialists offer the latest evidenced-based treatments and therapies, and have a range of clinical studies available – designed to provide patients the most accessible care leading to best patient outcomes. We take pride in offering individual, personalized care to get you back to doing what you love most.
To schedule an appointment, please call the UC Health IBD team
- 513-475-7505Compassionate Healing Starts Here
Click below to learn more about where you can find compassionate care.
ABOUT THIS CONDITION
Understanding Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) represents a group of conditions characterized by chronic inflammation in the digestive tract. The two main forms of IBD are ulcerative colitis and Crohn's disease. Although both conditions are under the IBD umbrella, they affect the body in different ways.
Ulcerative colitis is confined to the colon and rectum, where it causes ulcers and inflammation. Crohn's disease can affect any part of the gastrointestinal tract, from the mouth to the anus, and the inflammation can spread deep into the tissue layers.
Understanding the Basics of IBD
The Digestive Tract: A Primer
At its core, the digestive tract is a complex system responsible for processing the food we eat, absorbing nutrients, and eliminating waste. It starts at the mouth, includes the esophagus, stomach, small and large intestines, and ends at the rectum and anus. Inflammatory Bowel Disease primarily affects the intestines, where most nutrient absorption occurs.
Key Differences: Ulcerative Colitis vs. Crohn’s Disease
While both ulcerative colitis and Crohn's disease are types of IBD, they have distinct differences:
Ulcerative Colitis affects only the colon and rectum. It causes continuous damage to the lining of the colon, leading to ulcers and inflammation.
Crohn’s Disease can occur anywhere in the digestive tract, from the mouth to the anus, and often impacts the entire thickness of the bowel wall. This can lead to complications beyond inflammation, including blockages and fistulas.
Chronic Inflammation and Its Role in IBD
Chronic inflammation in IBD can lead to various symptoms and complications. Inflammation is the body's response to injury or irritation, but in IBD, this response is improperly activated, leading to damage in the digestive tract. Understanding and managing this inflammation is key to treating IBD and improving the quality of life for those affected.
Causes and Risk Factors
The Complexity of IBD Causes
Inflammatory Bowel Disease (IBD) is the result of a complex interplay of factors that contribute to its onset and progression. Understanding these can help manage the condition more effectively.
- Genetic Predispositions: Family history plays a crucial role. Individuals with a family member diagnosed with IBD are at a higher risk, indicating genetics are a significant piece of the puzzle.
- Environmental Factors: Lifestyle choices and environmental exposures, including diet, smoking, and possibly stress levels, can influence the risk of developing IBD.
- Unusual Immune Reactions: At the heart of IBD is an immune system that reacts inappropriately, mistaking benign or beneficial cells and bacteria in the gut for harmful invaders, leading to inflammation.
- Imbalance in Gut Bacteria: A healthy gut microbiome is essential for digestive health. In people with IBD, there's an imbalance with too many harmful bacteria and not enough beneficial ones, contributing to inflammation and symptoms.
Symptoms and Diagnosis
Recognizing IBD Symptoms
The symptoms of Inflammatory Bowel Disease (IBD) can vary significantly between individuals and over time, reflecting the chronic, often fluctuating nature of the conditions.
Common Symptoms Shared by Ulcerative Colitis and Crohn’s Disease:
These include persistent diarrhea, abdominal pain and cramping, blood in the stool, reduced appetite, and unintended weight loss. These symptoms can range from mild to severe and may come and go in cycles of flare-ups followed by periods of remission.
Specific Symptoms for Ulcerative Colitis
These involve ulceration and bleeding of the colon's lining, leading to bloody stools and urgency in bowel movements.
Specific Symptoms for Crohn’s Disease
This can include more severe complications due to the disease's ability to affect the digestive tract's entire thickness. These complications might be fistulas, abscesses, and blockages in the intestine.
Diagnostic Approaches
Diagnosing IBD involves a combination of tests and procedures to rule out other potential causes of symptoms and to determine the presence and extent of the disease.
- Laboratory Tests and Imaging: Blood tests can check for anemia or infection, while stool tests can look for blood or signs of inflammation. Imaging tests, like CT scans and MRI, can provide detailed pictures of the entire digestive system.
- Endoscopic Procedures and Biopsies: Colonoscopy and gastroscopy allow doctors to see the lining of the digestive tract directly and to take tissue samples (biopsies) for examination. These procedures are critical for diagnosing IBD and differentiating between ulcerative colitis and Crohn’s disease.
- Differentiating IBD from Irritable Bowel Syndrome (IBS): Although IBS shares some symptoms with IBD, such as abdominal pain and diarrhea, it does not cause inflammation, ulcers, or other damages to the bowel tissues. A correct diagnosis is essential for effective treatment.
Treatment and Management
IBD Treatment Overview
The treatment of Inflammatory Bowel Disease (IBD) aims to reduce inflammation that triggers symptoms, with the ultimate goals of achieving remission and preventing flare-ups. Since IBD varies greatly among individuals, treatment plans are highly personalized.
- Medication Strategies: Managing Inflammation and Symptoms: Medications are the cornerstone of IBD treatment, including anti-inflammatory drugs, immune system suppressors, antibiotics, and biologic therapies. These medications can help reduce inflammation, heal the intestine, and relieve symptoms.
- Surgical Options for Severe Cases: Surgery may be necessary for those with complications or when other treatments haven’t been effective. For ulcerative colitis, this might involve removing the entire colon. In Crohn’s disease, surgery can remove damaged portions of the digestive tract or repair blockages.
The Role of Diet and Lifestyle Changes
While medications are essential, diet and lifestyle adjustments play a crucial role in managing IBD symptoms and maintaining remission.
- Diet: No single diet works for everyone with IBD, but certain foods and drinks can exacerbate symptoms. Patients are often advised to follow a balanced diet and possibly avoid dairy, high-fiber foods, or other known irritants during flare-ups. Nutritional support or supplements might be necessary for those with specific deficiencies. Here is a more in-depth guide to IBD Diet recommendations.
- Lifestyle Changes: Stress management techniques, regular exercise, and quitting smoking can all positively impact IBD management, helping reduce flare-ups and improve overall well-being.
Advances in IBD Treatment
The field of IBD treatment is rapidly evolving, with ongoing research into new medications, therapies, and even the potential for personalized medicine based on genetic profiles.
- Clinical Trials and Emerging Therapies: Participation in clinical trials can provide access to cutting-edge treatments. Emerging therapies, including new biologic drugs and cell therapies, are focusing on more targeted ways to treat IBD.
- The Promise of Personalized Medicine in IBD Care: Advances in understanding the genetic and microbial factors in IBD are paving the way for personalized treatment plans. These approaches aim to tailor therapies based on individual patient profiles, potentially improving effectiveness and reducing side effects.
Effective management of IBD requires a comprehensive approach, combining medical treatment with dietary and lifestyle adjustments. Ongoing communication with healthcare professionals is vital to adapt the treatment plan as needed and to navigate the challenges of living with IBD.
Living with IBD
Living with Inflammatory Bowel Disease (IBD) involves more than just managing symptoms; it's about maintaining a quality of life that feels fulfilling and active. Here's how individuals with IBD can navigate daily life effectively.
Managing Everyday Life
- Nutritional Considerations and Dietary Guidelines: A balanced, nutritious diet is crucial. While there's no one-size-fits-all diet for IBD, monitoring how certain foods affect your symptoms can guide dietary choices. Keeping a food diary may help identify triggers. Nutritional supplements might also be recommended by healthcare providers to address specific deficiencies.
- Lifestyle Adjustments for IBD Patients: Regular exercise, adequate sleep, and stress reduction can significantly impact well-being. Activities like walking, yoga, or meditation can help manage stress and contribute to overall health. It's also important to build a support system of friends, family, and healthcare professionals who understand IBD.
Coping with IBD: Mental and Emotional Health
- Mental Health Support: Living with a chronic condition like IBD can be challenging mentally and emotionally. Seeking support from a mental health professional can be beneficial. Many find comfort and understanding in support groups, whether online or in-person, where they can share experiences and strategies with others who understand the reality of IBD.
- Educating Yourself and Others: Understanding your condition empowers you to make informed decisions about your health. Additionally, educating those around you about IBD can foster a supportive environment and reduce misunderstandings related to the disease.
Living with IBD requires adapting to the condition's demands while striving to lead a life that's as normal and active as possible. With the right strategies and support, individuals with IBD can manage their symptoms and enjoy a good quality of life.
Research and Future Directions
The Frontiers of IBD Research
As we venture further into Inflammatory Bowel Disease (IBD) research, new horizons are emerging that promise to reshape our understanding and treatment of these conditions. Key areas of focus include:
- Latest Findings in Gut Microbiome Studies: The complex ecosystem within our digestive system, known as the gut microbiome, plays a crucial role in IBD. Recent studies have shown that imbalances in gut bacteria may not only trigger IBD but could also influence the severity of the disease. Research is now exploring how manipulating the microbiome through diet, probiotics, and even fecal microbiota transplants could offer new treatment avenues.
- Genetic Research and Its Implications: With hundreds of genes identified that are linked to an increased risk of IBD, genetic research offers greater understanding into why IBD develops in some individuals and not others. This knowledge is paving the way for genetic testing to predict susceptibility to IBD, understand individual patient responses to treatments, and develop targeted therapies.
- Innovations in Treatment and Management Strategies: The future of IBD treatment lies in personalized medicine. By combining genetic, microbiomic, and clinical data, researchers are working towards tailored treatment plans that maximize efficacy and minimize side effects. New drug developments, including small molecule drugs and advanced biologics, are focusing on specific pathways and molecules involved in the inflammatory process.
Contributing to IBD Research
For those living with IBD or their loved ones, contributing to ongoing research can be a powerful way to fight back against the disease.
- Participating in Clinical Trials: Clinical trials offer patients the opportunity to access the latest treatment innovations before they are widely available. Participation not only helps individuals potentially find more effective treatments but also contributes valuable data that can advance research for all those affected by IBD. Discover clinical trials here.
- Supporting IBD Research Initiatives: Financial contributions to research foundations and institutions are crucial for advancing IBD research. Funding supports everything from basic science studies to large-scale clinical trials. Volunteering time or participating in fundraising events can also make a significant impact.
As we look to the future, the ongoing collaboration between patients, researchers, and clinicians is essential for continuing to make strides in understanding and treating IBD. With each new discovery and innovative treatment, we move closer to a world where IBD can be effectively managed or even cured.
Contact Us
At UC Health, we lead the region in scientific discoveries and embrace a spirit of purpose – offering our patients and their families something beyond everyday healthcare. At UC Health, we offer hope.