Managing Symptoms Through Diet
Diet plays a critical role not just in managing flare-ups but also in maintaining remission and overall well-being for those with IBD. It's about finding a balance that nourishes the body without triggering symptoms.
Physician Insight on Symptom Management
"During times of active disease, it is important to focus on small portions every few hours if larger meals are not tolerable and consider oral nutrition supplements if you have trouble meeting your nutrition needs. Keeping a food journal can also help track your symptoms and identify your personal food triggers."
Gradually Reintroducing Foods
Once symptoms are under control, gradually reintroducing foods into your diet can help widen the variety of nutrients consumed and identify any specific food sensitivities. This process should be done methodically, with careful monitoring of symptoms, ideally under the guidance of a healthcare provider or dietitian.
Limiting Problematic Foods Even in Remission
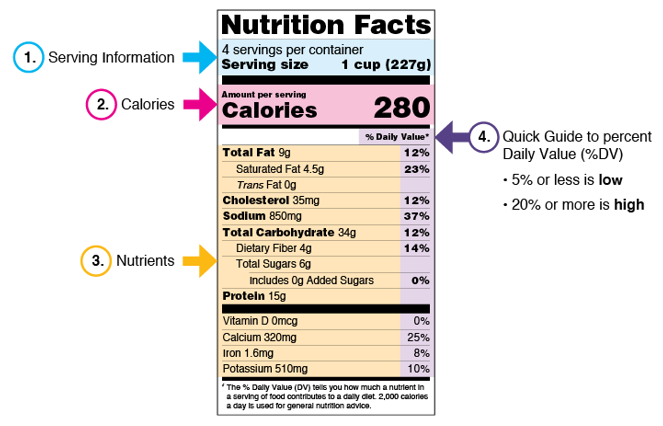
Some foods may need to be limited long-term, including those high in added sugars and saturated fats. Continuing to focus on a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats—similar to the Mediterranean diet—is advisable even when symptoms are not present.
We hope you are feeling better!
Managing IBD through diet requires a personalized approach, with an emphasis on avoiding trigger foods, incorporating nutrient-dense snacks, and maintaining a balanced diet to support overall gut health. Working closely with healthcare professionals, including registered dietitians, can provide tailored advice and support to navigate the complexities of nutrition for IBD.
Remember, while diet plays a crucial role in managing IBD, it's just one part of a comprehensive care strategy that includes medication, stress management, and regular medical check-ups. By paying close attention to your body's responses to different foods and adjusting your diet accordingly, you can take an active role in managing your IBD and improving your quality of life.