What kinds of treatment are available for hearing loss?
Over 30 years ago, UC Medical Center was the first in the region to offer cochlear implants for severe hearing loss. As a national center for treating ear and cranial base disorders, we offer patients unparalleled expertise and a personalized approach at several convenient locations.
Among the treatments we offer are:
- Personalized hearing treatments. Many causes of hearing loss are not permanent. By working to find the exact reason for hearing loss for each individual, our experts in hearing could offer medical and surgical treatments to improve natural hearing.
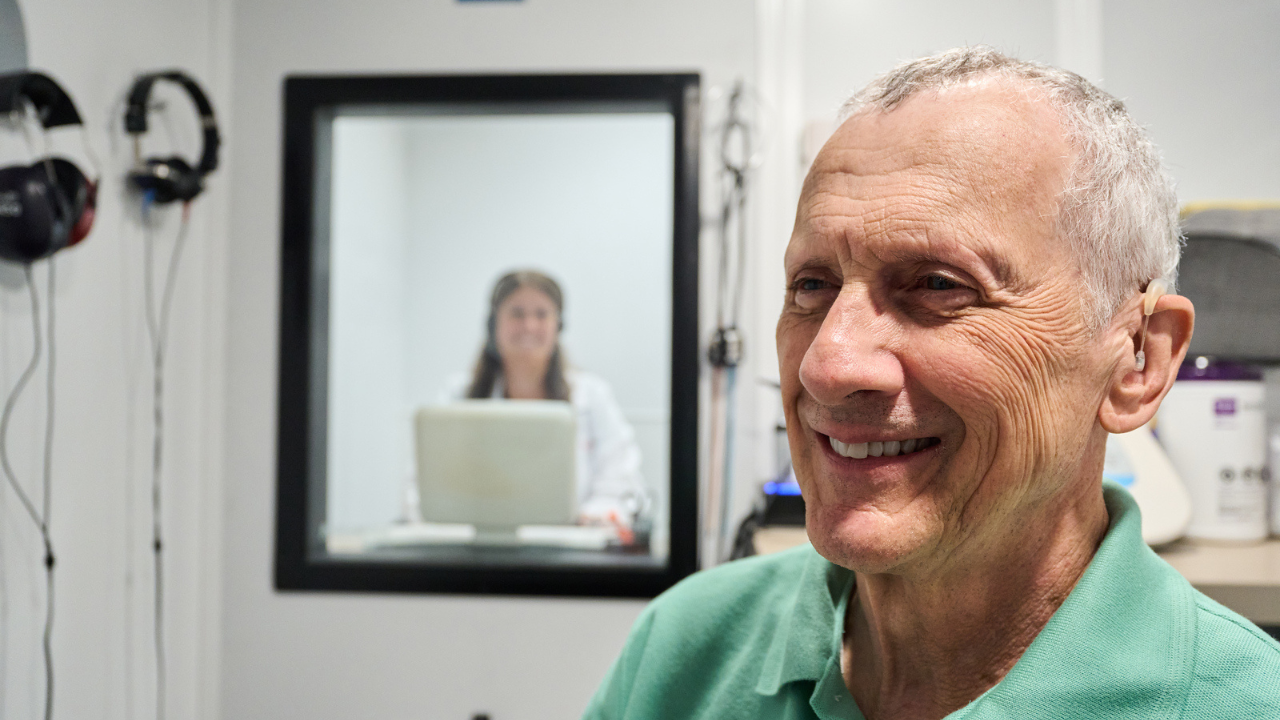
- Hearing aids. These small, electronic devices are worn in or behind the ear to amplify sound and improve hearing for people with hearing loss. The advanced technology of hearing aids includes features like reducing background noise, directional microphones that make it easier to hear in noisy environments, and wireless connectivity, so you can stream audio from phones, TVs and other devices. Our experts work with you to find a hearing aid system that best suits your needs and lifestyle.
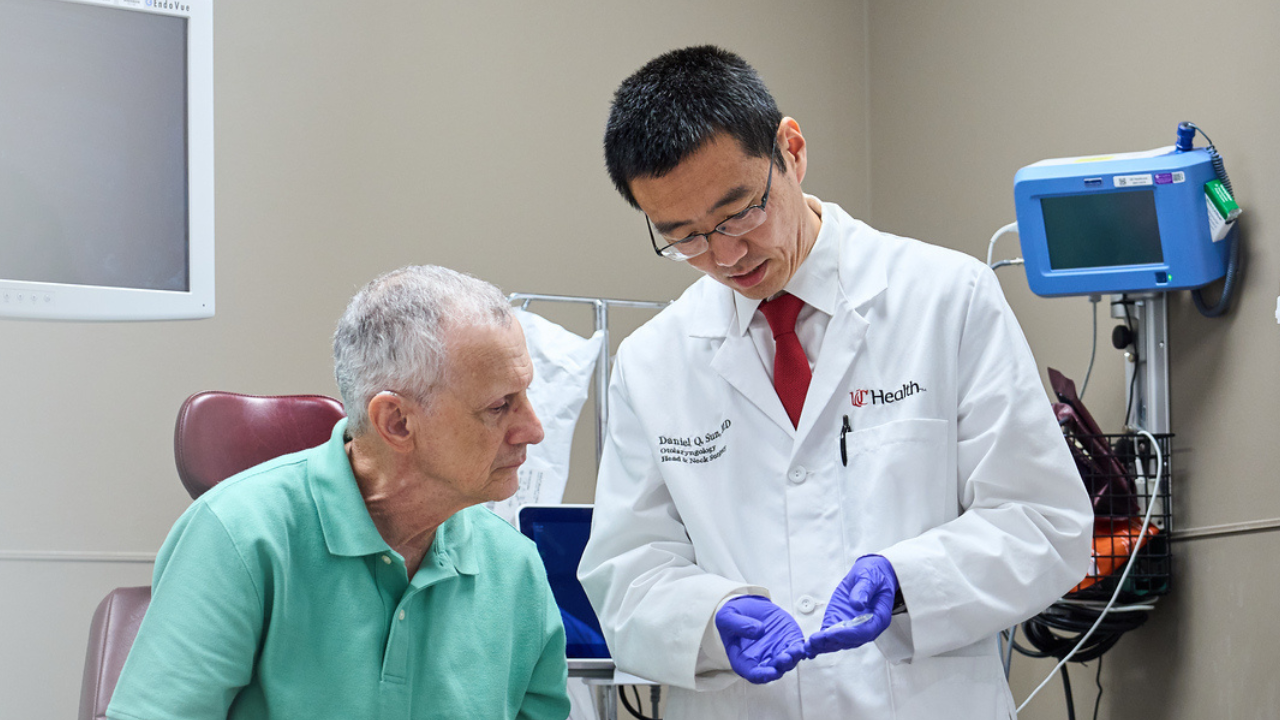
- Cochlear implants. These electronic devices are surgically implanted in the inner ear to restore or improve hearing in people with severe hearing loss for whom hearing aids are no longer sufficient.
- Bone-anchored hearing aids, bone conduction implantable hearing devices and bone-anchored auditory implants. These systems bypass the outer and middle ear by conducting sound through bone, directly to the inner ear. They’re typically used for conductive hearing loss, single-sided deafness, mixed hearing loss and cases where traditional hearing aids aren’t suitable.
We understand that there’s no one treatment that fits everyone. By blending leading-edge research with personalized care, we put you at the center of a collaborative, multidisciplinary team focused on finding what’s right for you.
Do UC Health and the University of Cincinnati conduct research?
As a leading academic health system, our teams conduct advanced and groundbreaking research into hearing loss. Our research programs include ongoing clinical trials focused on bringing new therapies and diagnostic tests to patients around the world.
As a research center, our patients have access to clinical trials and promising new treatments.
National Speech-Language-Hearing Month is also a time to celebrate our team
May is also the perfect time to recognize the incredible work done by our audiologists, SLPs and the other dedicated experts who help patients across Greater Cincinnati and Northern Kentucky speak, hear and live more fully.
At UC Health, our audiology and speech-language pathology professionals are more than providers; they’re educators, collaborators and innovators, leading the way in diagnosis, treatment and rehabilitation.
Hearing and balance: expertise rooted in compassion
Our audiology team provides the most comprehensive testing available in the region, using advanced technology to diagnose hearing loss and balance disorders with unmatched accuracy. But their impact goes far beyond diagnostics.
These professionals work with UC Health otolaryngologists, community ear, nose and throat physicians and other medical experts to identify the root cause of hearing and balance issues and, more importantly, find a solution that restores confidence and well-being.
Whether treating dizziness, tinnitus or severe hearing loss, our audiologists bring decades of expertise and a personal touch to every patient interaction. Their dual role as care providers and educators also ensures the next generation of audiologists is being trained right here at UC Health.
Speech-language pathology: helping patients reclaim their voices
Our SLP team supports patients who are re-learning how to speak, communicate, swallow and think clearly after an injury, illness or surgery. Their expertise spans stroke, brain injury, neurological disorders (like Parkinson’s disease, multiple sclerosis and ALS) and tracheostomy and ventilator care.
Through comprehensive evaluations and personalized treatment plans, our SLPs help patients regain everyday functions that many of us take for granted. This includes:
- Speech and cognitive rehabilitation to improve problem-solving, memory and communication
- Swallowing therapies using advanced diagnostics like modified barium swallow study, fiberoptic endoscopic evaluation of swallowing and VitalStim therapy
- Device evaluations for augmentative and alternative communication, tailored to each patient’s unique needs
Southwest Ohio’s only voice and swallowing center of excellence
UC Health offers the region’s only specialized program for patients dealing with complex swallowing, airway and voice disorders. Led by fellowship-trained laryngologists and specialty-trained SLPs, our multidisciplinary teams bring together experts from neurology, gastroenterology, pulmonology, physical therapy and more to provide world-class care, all at one center.
Whether a patient is recovering from throat cancer, struggling with vocal cord dysfunction or facing lifelong swallowing challenges, our team uses the latest research to provide innovative, compassionate treatment that restores quality of life. Watch how our dysphagia team is making a difference.
Thank you to our speech-language-hearing professionals
This May, we extend our deepest gratitude to the audiologists, SLPs, assistants, and all supporting team members who work tirelessly to restore essential functions and improve lives. Your commitment to excellence, education, and patient-centered care is what makes UC Health a leader in this field and a beacon of hope for those we serve.
Happy National Speech-Language-Hearing Month!