Atrial fibrillation (AFib) can be stubborn—especially in its persistent or long-standing forms. That’s where the hybrid AF convergent procedure offers new hope.
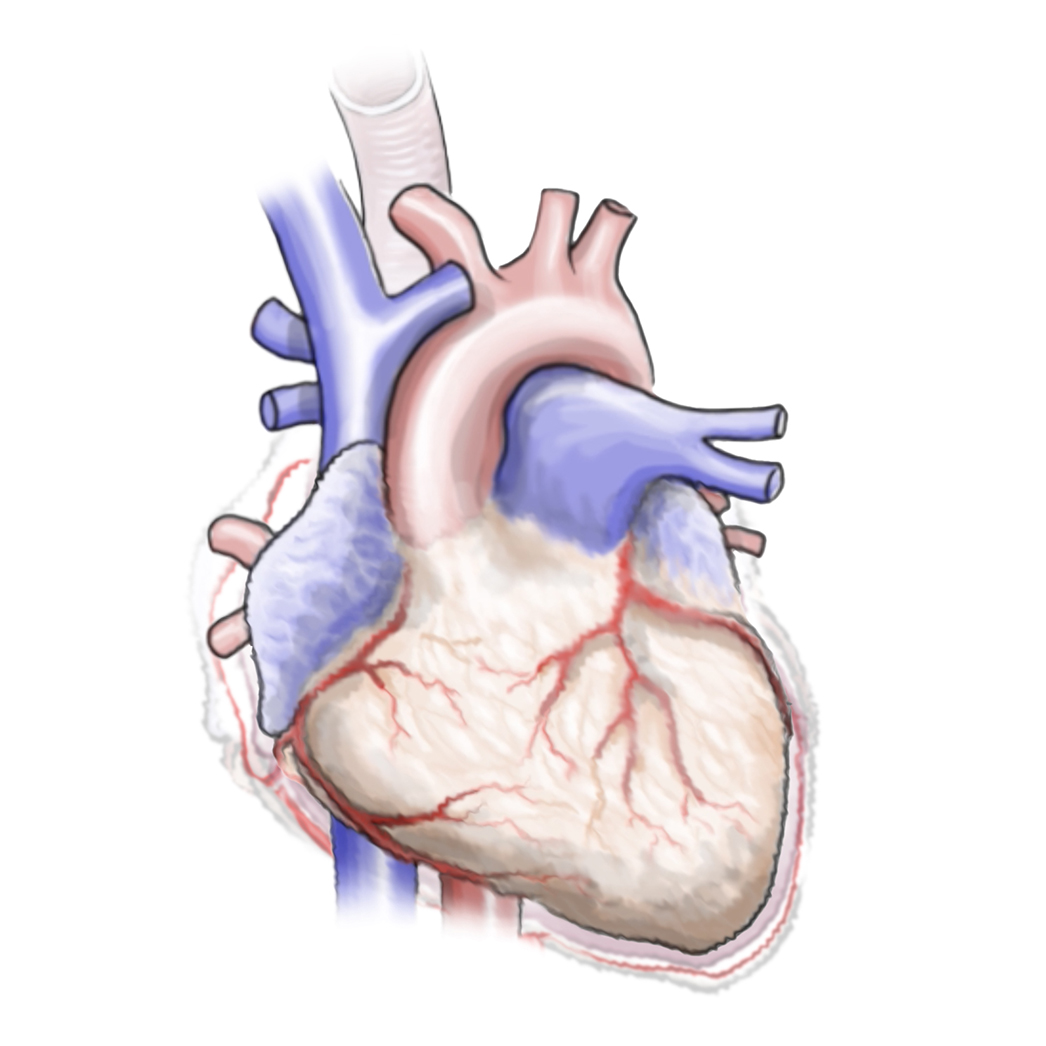
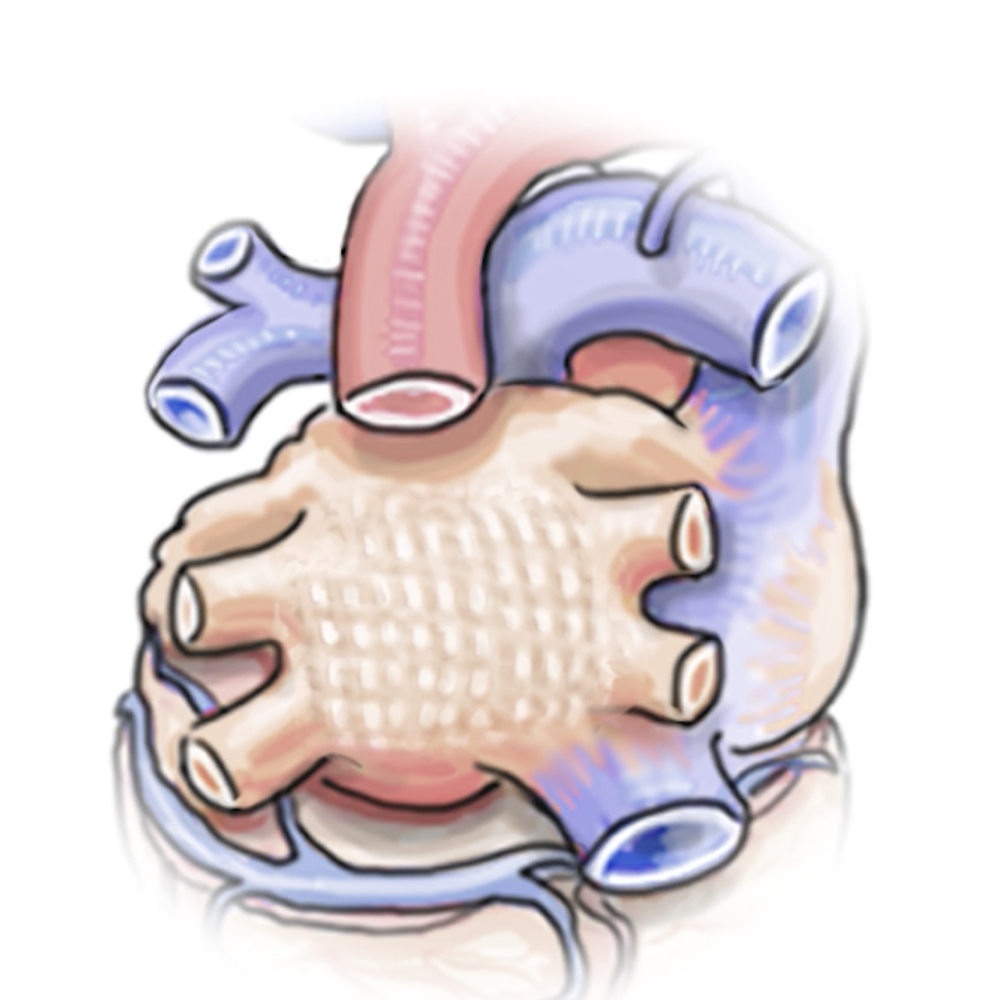
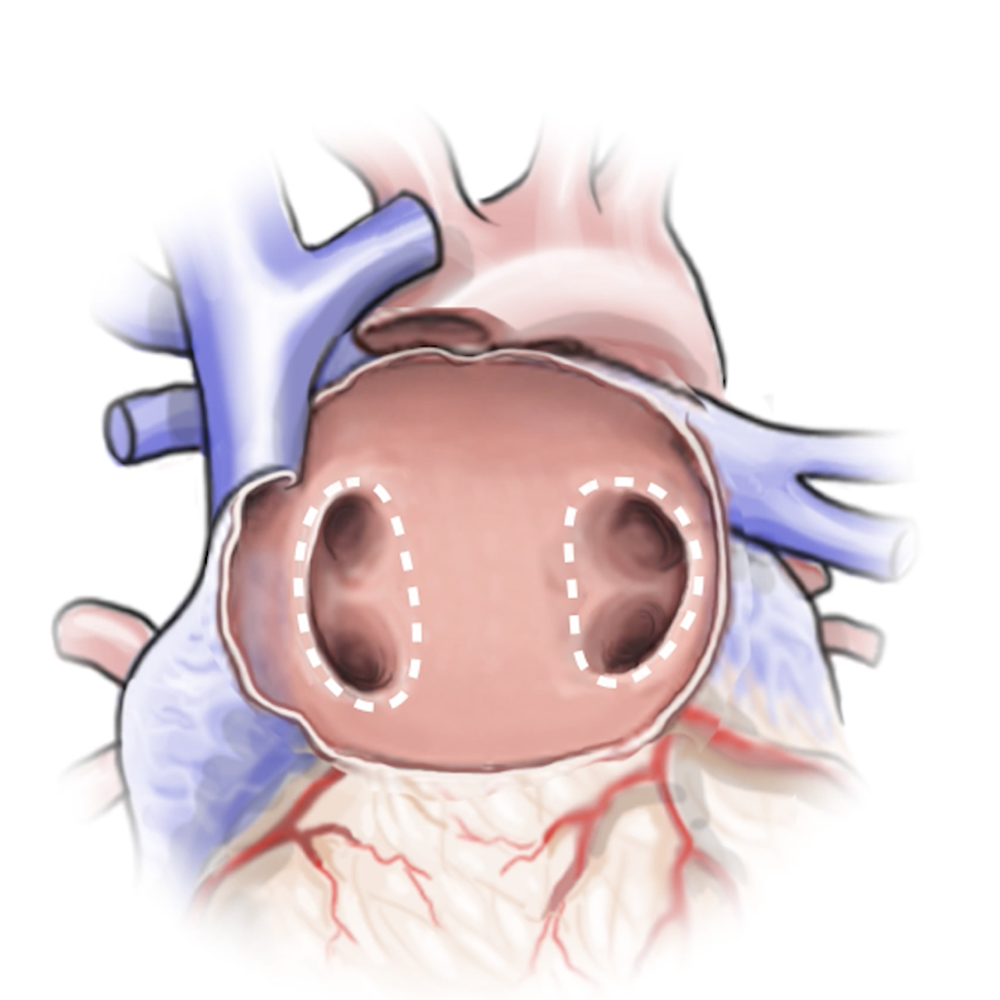
At UC Health in Cincinnati, this innovative treatment brings together two specialized cardiovascular teams, cardiac surgeons and electrophysiologists, to address AFib from both the outside and inside of the heart. By combining a minimally invasive surgical technique with a catheter-based ablation treatment, the procedure reaches more of the heart tissue responsible for irregular rhythms.
The goal is to restore and maintain a healthy, steady heartbeat while reducing stroke risk and improving long-term outcomes. This dual approach combines precision, teamwork, and personalized care that adapts to the complexity of your condition.