Critical Care Use of Aviation Training Principles
Various strategies are employed at hospitals and health systems to reduce medical errors and improve patient safety, with some adopting aviation protocols, another industry with a high risk environment. Renee Hebbeler-Clark, MD, MS, director of patient safety education for graduate medical education at University of Cincinnati Medical Center, oversees training programs to ensure that 650+ residents learn the value of teamwork and communication in achieving better patient outcomes. According to Hebbeler-Clark, aviation and patient safety first crossed over in anesthesia, and common tactics have been identified that specifically benefit the critical care environment, a complex, high-risk, and stressful setting.1
One gap Hebbeler-Clark identified was in skills and refresher training. She noticed that competency training was not required for physicians after board certification, whereas in aviation, pilots recertify in a simulator every six months. In response to this, in 2013, she piloted an “Acute Care Boot Camp,” which takes place entirely in a simulated environment. By enabling interns and residents to become familiar and comfortable with the team dynamic required in acute care medicine, she hopes to ensure their ability to make effective contributions to patient care from their first day “on the floor.” At the end of the program, participants are tested on their rapid response skills including identifying patient emergencies, maintenance of detailed check sheets, inserting a central line, and using sterile technique, to name a few.
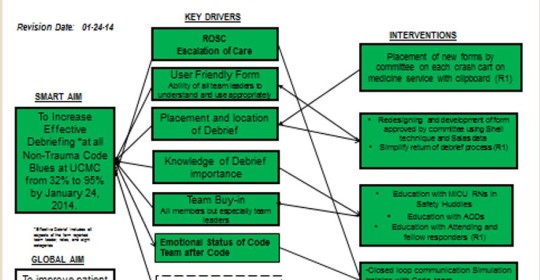
Key drivers used in “Team CoDe”: Counting on Debriefs: Improving Debriefs after Non-trauma Codes: A Quality Improvement initiative at a University Medical Center: Utilization of a Multidisciplinary Debrief Tool.
Current initiatives also include the “Team CoDe” program, which was implemented because ICU staff were not consistently performing debriefs. The initial rate of debriefs completed was 35%.2 At month three of the project, the rates were 75%, and by the project’s end, rates exceeded 95%.2 These improvements were sustained during the six-month follow up period.2
According to Hebbeler-Clark, aviation-based programs have become more prevalent in academic medical centers, which emphasize human-factors divisions and the importance of team-based medicine. In several respects, however, medical safety processes have begun to diverge. For example, unlike aviation work environments where the focus is typically on the collective safety of passengers on a single flight, ICUs consist of large medical and nursing teams that care for multiple patients simultaneously.1 Problem solving is key, and teams must diagnose poorly understood patient illnesses, stabilize the condition of patients, and stimulate recovery.1 Hebbeler-Clark points out the key factor that unites the two disciplines and underscores the importance of team-based training: “Safety, whether of patients or passengers, is everybody’s responsibility.”
References: 1. Reader TM and Cuthbertson BH. Teamwork and team training in the ICU: Where do the similarities with aviation end? Critical Care 2011, 15:313:1-6. 2. Hebbeler-Clark R, Schlinkert A, Smith BJ, and Williams K. “Team CoDe”: Counting on Debriefs: Improving Debriefs after Non-trauma Codes: A Quality Improvement initiative at a University Medical Center: Utilization of a Multidisciplinary Debrief Tool (265). Poster presented at the Society of Critical Care Medicine annual meeting, February 2015.
Renee Hebbeler-Clark, MD, M.S.
Assistant Professor of Clinical Medicine, Critical Care Medicine and Infectious Diseases
Director Patient Safety Education, Graduate Medical Education
(513) 558-2924
hebbelers@ucmail.uc.edu


