An Aortic Center with Aggressive Aortic Rupture/Trauma Protocol: The Minutes That Can Save a Life
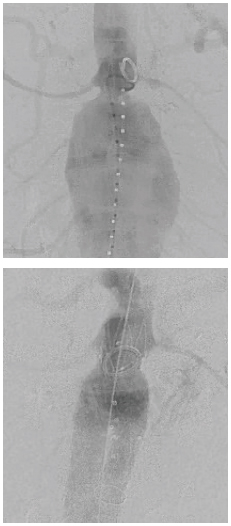
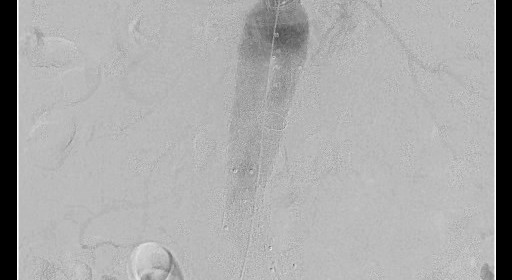
An 82-year-old male with multiple medical problems was transferred from a community hospital with a ruptured large abdominal aortic aneurysm. He was deemed inoperable at the other hospital. He arrived to the University of Cincinnati Medical Center hybrid angiographic suite and was treated with an endovascular repair of his aortic aneurysm. (Above: Pre-intervention, Below: Post-repair).
Endovascular repair of ruptured aortic aneurysms or aortic trauma repair has become the standard of care in recent years, overtaking the traditional open approach. This is secondary to both improved survival rate and less morbidity of this minimally invasive approach as compared to the open procedure. According to Amit Jain, MD, director of University of Cincinnati Medical Center’s newly launched Aortic Center, to be formally dedicated sometime in 2015, “For a patient with a ruptured or transected aorta, time means life, and a protocol-based approach has shown to improve outcomes.”1
All hospitals in the Cincinnati, Ohio region send patients with an aortic aneurysm rupture or traumatic injury to the University of Cincinnati Medical Center, usually via Life Flight helicopter. Jain explains, “We’ve developed a very aggressive protocol for these cases. When the patient lands at the helipad, they completely bypass the emergency room and within a few minutes after arrival, the patient is directly transported to the operating room. In the operating room, there is a team of vascular surgeons, anesthesiologists, nurses and X-ray technicians available and on call 24/7, ready to treat this patient. This contrasts with the more common scenarios, seen in most other hospitals, where patients are first evaluated in the ER, delaying OR entry.”
At the University of Cincinnati Medical Center Aortic Center, all such patients first undergo endovascular aortic balloon occlusion to achieve hemodynamic stability. This procedure is accomplished expeditiously under local anesthesia within minutes of their arrival in the OR. The vascular surgical team then performs an angiogram, followed by endovascular repair if the patient’s aortic anatomy is appropriate. Occasionally, cases convert to an open approach. Jain reports that the team performs an average of five to eight such emergency aortic repairs each month and adds, “Since instituting this more aggressive protocol, we’ve seen a real decrease in mortality in accordance with the published literature of about 80% survival.2 For excellent results, it’s equally important to have a good critical care team that manages these patients pre-, intra- and post-operatively.” To successfully address a wide variety of trauma presentations, it is also key that surgeons have experience in performing both endovascular and open procedures. A major challenge going forward will be to ensure that the next generation of vascular surgeons remains well-trained in performing open surgeries as well.
University of Cincinnati Medical Center is a level 1 trauma center and serves as a referral center for a large number of community medical centers across the states of Ohio, Kentucky and Indiana. Jain explains, “The patients involved in traumatic events like car accidents can sometimes have subtle injury to the inner lining of their thoracic aorta that could be overlooked at initial presentation but can present weeks to months later with aneurysmal degeneration. Hence, all such patients should be followed at a dedicated vascular center with CT scan angiography to ensure stability of their initial small intimal injury.”
Jain and colleagues are also performing complex non-emergent thoracic and abdominal aortic aneurysm and dissection repairs. He explains, “In order to reduce the number of surgical operations these patients undergo, we’ve been performing a larger number of hybrid repairs, where two different repairs are performed at a single time with simultaneous use of open and endovascular approaches.” While somewhat more complex, hybrid surgeries decrease risks for pulmonary and hemodynamic instability, as well as reduce recovery time and hospital resource usage. Jain notes, “The Aortic Center is fortunate to have a vascular surgical team with a wide breadth of expertise, including endovascular, open and laparoscopic repair techniques. In this way, we can flexibly handle any cases that present to us using a variety of treatment approach options.”
George H. Meier, MD, RVT FACS, professor, chief, and program director of vascular surgery, concludes, “This approach to the management of critical thoracic and abdominal aortic pathology is only available at a few sites nationally, of which the University of Cincinnati Medical Center is the only one regionally. Our system of aggressive care truly makes a lifesaving difference in many of these patients’ lives.”
Amit Jain, MD
Assistant Professor of Surgery
Division of Vascular Surgery
Director, Aortic Center, University of Cincinnati Medical Center
(513) 558-5146
amit.jain@uc.edu

