Radiofrequency Catheter Ablation in Heart Failure Patients with Atrial Fibrillation More Effective than Medication
According to Alexandru Costea, MD, radiofrequency catheter ablation can be more effective than the standard, current treatment of antiarrhythmic medications in patients with atrial fibrillation (AF) and heart failure (HF). It is well known that in patients with AF but not HF, the benefits of radiofrequency catheter ablation are significant, with success rates ranging from 70% to 80% in experienced centers, such as the University of Cincinnati (UC) Medical Center. With the most effective medications, the chance of patients staying in normal rhythm after five years is only 60%, says Dr. Costea, professor of medicine, and director, Center for Electrophysiology, Rhythm Disorders and Electro-Mechanical Interventions, at UC Heart, Lung and Vascular Institute, Atrial Fibrillation Center.
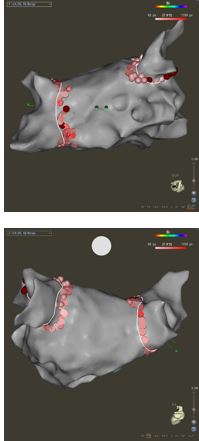
Images show pulmonary vein isolation using the Biosense Webster 3D mapping system and intracardiac ultrasound, automated lesion generation with Visitag Software. This procedure was done entirely without fluoroscopy. Images courtesy of Alexandru Costea, MD.
Dr. Costea’s experience is supported by a report at the European Society of Cardiology meeting of the CASTLE-AF clinical trial that studied radiofrequency catheter ablation or usual drug treatment in 363 subjects with temporary or persistent AF and HF.1 Radiofrequency catheter ablation lowered hospitalization and mortality rates by 47% and 44%, respectively, results that Dr. Costea termed “very strong.”
UC Medical Center has extensive experience with using radiofrequency catheter ablation in AF patients, with Dr. Costea and his team performing 300 to 400 procedures annually. The chance of complications, such as stroke, atrioesophageal fistula, and pulmonary vein stenosis, ranges from 2% to 5%, depending on specific risk factors of each patient, one important predictor being the presence of HF. Several outcomes studies are currently underway at UC Medical Center and other sites, in conjunction with researchers at the University of Utah (a co-leader of the CASTLE-AF trial). The focus of clinical research revolves around pre-procedure evaluation and screening, shortening the procedure duration without compromising outcomes, minimizing the use of fluoroscopy and relying on 3D mapping systems and intracardiac ultrasound. Other trials in progress include a retrospective review of catheter type (low-flow versus high-flow) and the benefits resulting from employing novel technology.
Radiofrequency catheter ablation of AF atrial fibrillation is performed by a specialist in electrophysiology usually with general anesthesia support. Optimal care however “requires extensive inter-disciplinary collaboration and protocols, enhanced by a certain level of experience available only in a high volume medical center,” says Dr. Costea. UC Medical Center’s multi-disciplinary team consists of an HF team that stabilizes the patient before and after ablation, the anticoagulation team, cardiac anesthesiologist, imaging team from the new Sanghvi Center for Advanced Cardiovascular Imaging, nurses, technicians and the interventional group. Dr. Costea says UC Medical Center’s best practices include confirming that the patient is in the best possible condition (i.e., checking medications, especially HF drugs) before, during and post procedure, while employing state-of-the-art technologies for diagnosis and treatment.
Another recent development is the routine usage of ultrasound to guide venipuncture. As this process has become a standard procedure, the vascular complications decreased significantly. “We began this a year ago and have observed a significant reduction in groin and vascular complications,” Dr. Costea says. “This allows us to safely treat high risk patients, patients on anticoagulation or patients with an increased body mass index without the fear of creating hematomas or other bleeding complications. Moreover, ultrasound guidance will allow safe same-day discharge after ablations, as accidental arterial puncture will not occur.”
Dr. Costea emphasized that UC Medical Center’s use of mapping instead of fluoroscopy shortens procedure time and is safer for the patient and the operating team because of lower radiation exposure. Currently, patients are hospitalized overnight, but Dr. Costea is developing a protocol to eliminate the hospital stay.
Reference:
1. Catheter ablation versus standard conventional treatment in patients with left ventricular dysfunction and atrial fibrillation—CASTLE-AF. Presented by Marrouche N, European Society of Cardiology Congress, Barcelona, Spain. August 27, 2017.
 Alexandru Costea, MD
Alexandru Costea, MD
Professor of Medicine
Director, Center for Electrophysiology, Rhythm Disorders and Electro-Mechanical Interventions
University of Cincinnati Heart, Lung and Vascular Institute Atrial Fibrillation Center
PHONE: (513) 584-0297
EMAIL: costeaai@ucmail.uc.edu
Connect with Dr. Costea on Doximity
Leave a reply →
