
Monthly Clinic Provides Additional Prenatal Care for Women with Adult Congenital Heart Disease, Recovers Patients “Lost to Follow-Up”
Although more adults than children are living with congenital heart disease (CHD) because of advances in treatment and technology, this good news has a potential downside. Adults with CHD will experience complications as they age, yet only 39% continue to see a cardiologist, and most are “lost to follow-up.”1 For women in the latter category, pregnancy may be the way they return to care. And, for pregnant women with adult CHD, this can be crucial since cardiovascular disease (CVD) is one of the leading causes of pregnancy-related death in the United States,2 says Nicole Brown, MD, cardiologist at Cincinnati Children’s Hospital Medical Center and the University of Cincinnati Medical Center.
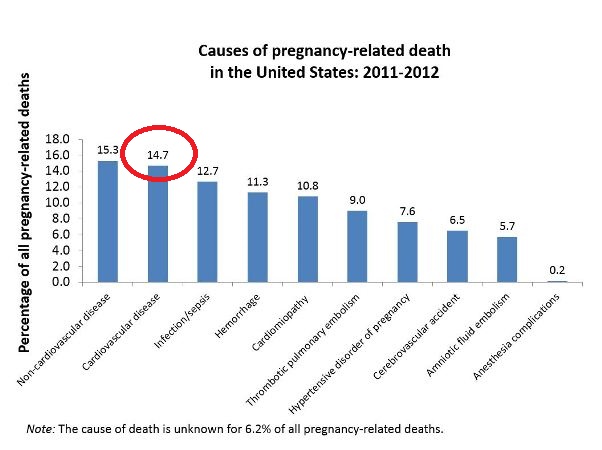
Cardiovascular disease accounts for 14.7% of pregnancy-related deaths in the United States. Image courtesy of the Centers for Disease Control and Prevention.2
Dr. Brown began a monthly clinic at the University of Cincinnati Medical Center in September 2015 for pregnant women with CHD. The management of this population is considered sufficiently complex that the Board of Medical Specialties created a new subspecialty in Adult CHD (ACHD). Dr. Brown and pediatric cardiologist Christopher Learn, MD are board-certified, having sat for the ACHD subspecialty boards in October 2015, when it was first offered.
Dr. Brown and her colleagues (three physicians, nurses and a social worker) staff the clinic and have completed care for five women; several more are still pregnant. The range of CV problems have included congenital heart defects with varying degrees of severity, pulmonary hypertension, connective tissue disease, and Marfan’s syndrome.
Ideally, Dr. Brown says “women with adult CHD should receive counseling before becoming pregnant from speaking with a high-risk obstetrician and cardiologist who have expertise in Adult CHD”. She pointed out that even the CV systems of pregnant women with normal hearts experience substantial changes – all the more reason for women with adult CHD to be identified and receive optimal care. Physicians perform an assessment to determine how pregnancy will affect a woman with CHD and then stratify her risk into low, medium or high categories for complications. The anticipated risk of a complication depends on the woman’s specific heart defect, the type(s) of heart repair she has undergone previously (the more complicated, the greater her risk during pregnancy), medications, heart-related signs, symptoms or events prior to pregnancy (or during a prior pregnancy), and how well the valves, heart muscle and lungs are functioning. Non-repaired CHD can pose a particularly high risk to women during pregnancy.
Risk assessment schemes include those from the World Health Organization – four rankings from no detectable risk to extremely high risk3 – and the CARPREG and ZAHARA I risk scores. In CARPREG, the additional risk of an adverse cardiac event during pregnancy is 27% if one risk factor is present, and the risk increases to 75% with two or more complications.4 Using the ZAHARA I risk score in a study of 1,802 women with Adult CHD,5 investigators found that arrhythmias (4.7%) and heart failure (1.6%) were the most frequent complications. According to Dr. Brown, other risks include volume overload, blood clots, and strokes. The risk to a developing fetus include low birth weight (14%), prematurity (12%) and death (4%).5
Dr. Brown emphasizes that even optimal care does not eliminate the potential for CV sequelae, stating “We ‘repair and palliate,’ not ‘cure and fix.’” Dr. Brown anticipates compiling and analyzing data from the recently opened clinic to help “close the clinical gap” by identifying, evaluating and treating pregnant women with ACHD.
Related Video: Dr. Brown and other UC physicians discuss congenital heart disease.
References:
- Mackie AS, Ionescu-Ittu R, Thierrien J, et al. Children and adults with congenital heart disease lost to follow-up: who and when? Circulation. 2009;120:302-309.
- Pregnancy mortality surveillance system. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PMSS.html#n7. Accessed February 22, 2016.
- Thorne S, MacGregor A, Nelson-Piercy C. Risks of contraception and pregnancy in heart disease. Heart. 92:1520–1525.
- Siu SC, Sermer M, Colman JM, et al, on behalf of the Cardiac Disease in Pregnancy (CARPREG) Investigators. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104:515-521.
- Drenthen W, Boersma E, Balci A, et al, on behalf of the ZAHARA Investigators. Predictors of pregnancy complications in women with congenital heart disease. European Heart Journal. 2010;31:2124-2132.
 Nicole M. Brown, MD
Nicole M. Brown, MD
Assistant Professor, UC Department of Pediatrics
Phone: 513-636-4432
E-mail: nicole.brown@cchmc.org


