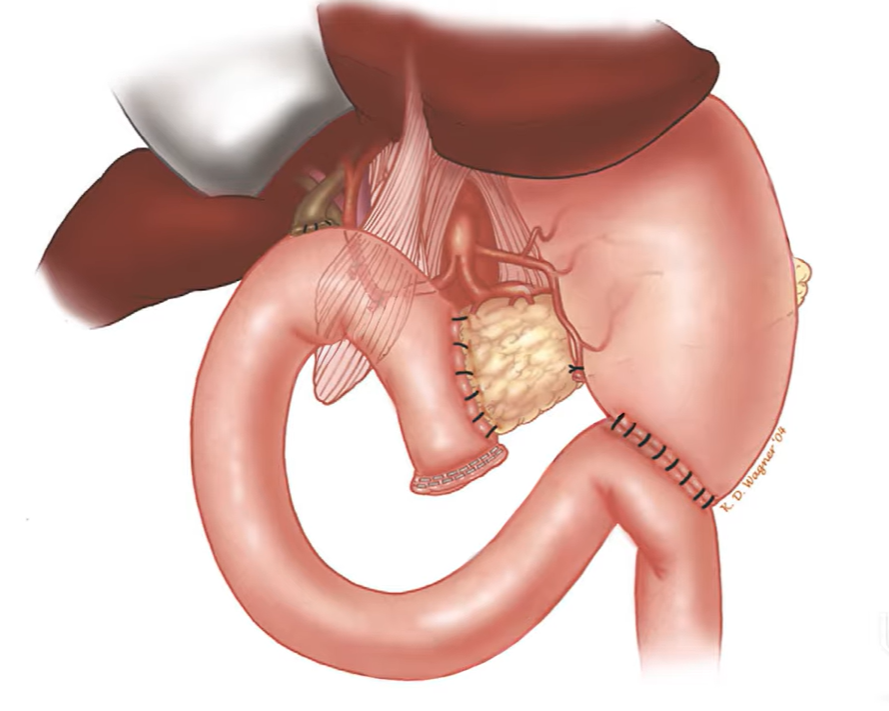
The Whipple proecedure, or Whipple surgery, is one of the most complex surgeries. It is often used to treat pancreatic cancer and other conditions affecting the pancreas, bile duct, or small intestine. In this video, experts from the University of Cincinnati Cancer Center break down the procedure in simple, easy-to-understand terms.
At the University of Cincinnati Cancer Center, our goal is to help patients and families feel informed, supported, and confident as they navigate care.