Understanding Your Risk for Breast Cancer
Breast cancer remains the most diagnosed cancer among women in the United States, touching the lives of millions and weaving a complex narrative of fear, hope, and resilience. In this intricate dance of cells gone awry, understanding one's personal risk factors becomes not just a measure of prevention but a step towards empowerment.
"Every woman should know their individual breast cancer risk! Breast Cancer affects one in eight women and some women are at even higher risk for developing the disease."
-Alicia Heelan, MD, MS, FSSO
At UC Health, we are dedicated to guiding you through this journey with our Breast Cancer Risk Assessment Program. This initiative isn't merely about identifying risks; it's about arming you with knowledge and actionable insights. Because when it comes to your health, knowledge isn't just power—it's protection.
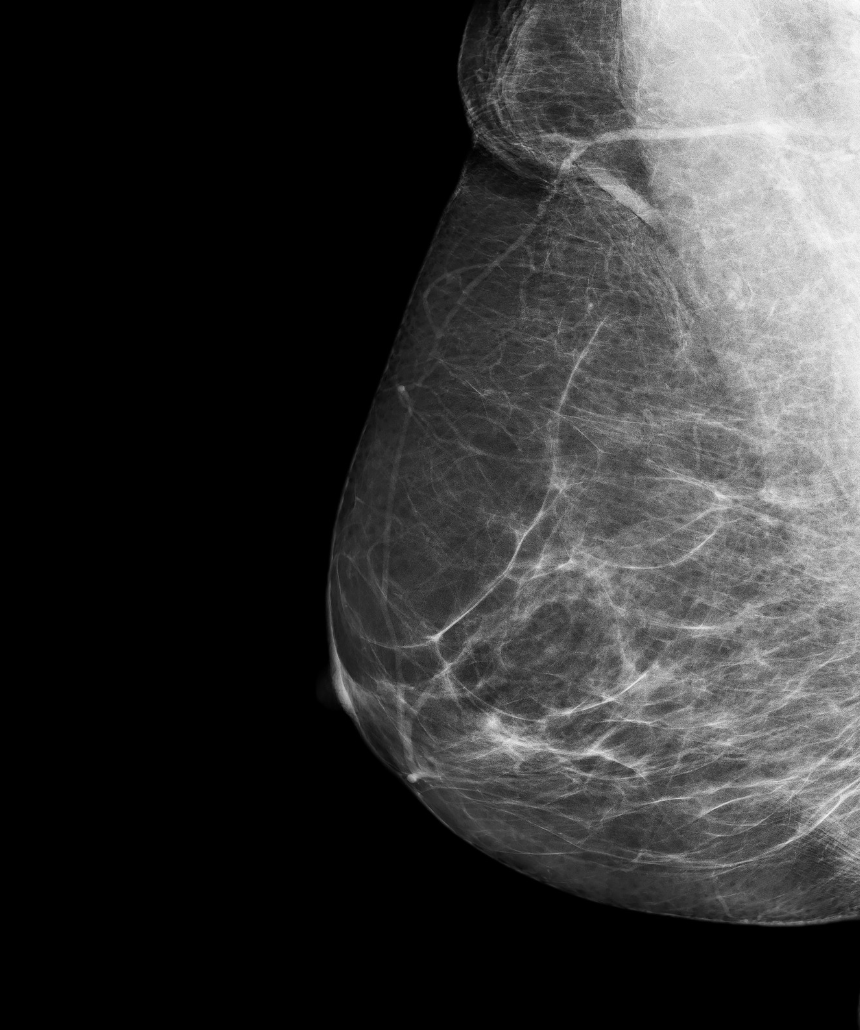
Navigating the waters of breast cancer statistics can feel overwhelming. Yet, amidst these numbers lies a beacon of hope: the power of early detection.
Studies have shown that catching cancer early can significantly improve treatment success rates. This is why understanding your risk, through both genetics and lifestyle factors, is a crucial step in taking control of your health narrative.
Let us walk you through this path of discovery, where each step taken is a move toward a healthier future. Because at UC Health, we believe in turning statistics into stories of survival and strength.
Key Highlights from this Guide:
Dive deeper into understanding your breast cancer risk and the comprehensive services offered by UC Health with these key sections of our guide:
- When More Than a Mammogram is Needed
- Recognizing Breast Cancer Symptoms
- The Major Risk Factors for Breast Cancer
- Breast Cancer Risk Assessment and Management Program (RAMP) Overview
- Breast Cancer Risk Factors Detailed
- High-Risk Factors and Prevention
- Genetic Testing and Counseling
- Engaging with Healthcare Providers
If you are interested in assessing your personal risk for breast cancer, continue reading and do not hesitate to reach out to us along the way with any questions you have.